See details
READ MORE
- General information about hip osteoarthritis
- Treatment of hip osteoarthritis
- Prevention of hip of hip of hip osteoarthritis
This article was written bt dr. Georgiana Tache, primary care physician, with over 30 years of experience, vicepresident of the Romanian Society of Rehabilitation Medicine.
General information about hip osteoarthritis
The most common cause of a joint disorder is the destruction of articular cartilage, which can develop into hip arthritis or hip osteoarthritis. The distinction between primary osteoarthritis with unknown causes and secondary osteoarthritis is made according to certain basic disorders (congenital malformations, rheumatism, circulatory disorders, accidents).Coxarthrosis is a fairly common disease, diagnosed mainly in patients in the middle age group and the elderly, as a degenerative-dystrophic pathology of the hip joint. Coxarthrosis, whose symptoms in the late stages of its course manifest itself as muscle atrophy of the affected area, combined with a shortening of the limbs, develops gradually over several years.
In the case of hip osteoarthritis, the joint loses its place more and more, bone deposits are formed along the edges, and the abrasion particles cause repeated pain. Cartilage loss results in increased joint stiffness. At the same time, pain occurs, being initially associated with movement after periods of inactivity and stress. Later, pain also occurs during the night and at rest, which leads to an increasing limitation of walking range and, finally, to a reduction in quality of life.
What is hip osteoarthritis?
Coxarthrosis is accompanied by painful sensations and limited mobility of the joints, and its causes can be very different. Although the lesion is found mainly in middle-aged and older patients (40 years and older), this disease can occur at an earlier age. Similar to many other conditions, hip osteoarthritis can be cured in the early stages of its manifestations, but many patients ignore the weak signs of the disease, which, if detected in time, can be cured without surgery.
The hip joint is made up of the femoral and ileal bones. Normally, the femoral head and acetabular cavity have a natural "lining" in the form of articular cartilage (hyaline). This lining has a considerable resistance and is at the same time smooth, and these characteristics determine the possibility of an ideal slip for the bones. Besides this ability, the articular cartilage in question acts as a shock absorber, effectively distributing the load that occurs during walking and movement.
Types of hip osteoarthritis
Coxarthrosis can be primary or secondary. The primary form of this disease develops under the influence of certain causes, and these can be considered only as hypotheses. The secondary form of coxarthrosis is because of other diseases that act as soil for its development (coxarthrosis is considered one of the symptoms of the disease against which it developed).Primary hip osteoarthritis
Primary hip osteoarthritis accounts for approximately 48% of all cases of this disease. This group includes patients in whom, despite a precise medical interview and clinical and radiological examination, the agent causing the disease cannot be clearly identified and the cause remains unknown.
Indirect factors that can affect the formation of hip osteoarthritis include the wrong lifestyle, environmental impact, and genetic predisposition. Studies have shown a correlation between the occurrence of hip osteoarthritis and the 16p chromosome, and the relationship between the Co19A1 gene located on the chromosome and the occurrence of osteoarthritis of the hip joint in women. This gene is associated with abnormal cartilage structure.
- congenital hip dysplasia
- acetabular roof hypoplasia
- deepening the acetabulum
- congenital or acquired hip dislocation
- abnormal development of the acetabulum during the growing period (Perthes disease, juvenile exfoliation of the femoral head)
- joint injuries after inflammation
- purulent or tuberculous process
- traumatic changes (for example, after a fracture of the femoral neck or trochanter of the femur, dislocation of the hip, jammed cartilage)
- overweight, obesity
- changes in overworked joints
- superimposed micro-traumas
- reduced resistance of the joint caused by osteoporosis
- hemophilia
- sub-active thyroid gland
- diabetes
- metabolic disorders or polyarthritis
The causes of secondary hip osteoarthritis are also related to changes in the blood source of the head and neck of the femur, as well as the properties of the blood.
Causes of hip osteoarthritis
Many hereditary diseases can lead to hip osteoarthritis. Usually, these are conditions that involve damage to connective tissue (ligaments, bones and joints) or collagen disease, for example, Stickler syndrome.Hip dysplasia is a congenital joint disease that originates in the underdevelopment of joint bones and ligaments, so some children often develop subluxations and dislocations of the femoral head. Some people may have dysplasia and don't even know it until they accidentally find it, for example, when they do an x-ray. These patients may develop osteoarthritis caused by dysplasia, a condition that occurs in women between the ages of 25 and 55. This is because reduced physical activity helps the joint to function normally. In young women, the disease can develop during pregnancy and after birth, and in mature and elderly people it happens after the decrease of physical activity after retirement.
Many diseases and conditions associated with metabolic disorders can affect blood supply and nutrition of articular cartilage. Unlike other tissues, the cells that produce the cartilage matrix - chondrocyte - do not get nutrients from the blood vessels, but directly from the synovial fluid. This is a very subtle biochemical mechanism that can be easily violated, which often happens.
Diseases such as diabetes, ochronosis, primary and secondary gout, hemochromatosis, Wilson's disease, and lack of sex hormones (estrogen) at menopause can lead to joint disorders. Because estrogen regulates metabolism in bones, ligaments, joints and, in general, in connective tissue, the lack of these hormones can become a trigger for the development of this disease.
Often joint injuries, which sometimes require surgery, contribute to hip osteoarthritis. After such events, the joint becomes a little "defective" (medically), and damage to the cartilaginous tissue of the joint can begin at any time.
The balance, like other parts and organs of our body, can be prone to inflammation. Inflammation of the joint (coxitis) can result from infection. In this case, the disease develops with massive damage to the articular cartilage, and recovery can take quite a long time and, as a result, secondary hip osteoarthritis can begin.

Risk factors for hip osteoarthritis
In addition to disorders in the structure and mechanics of the joint, the risk of degenerative changes in the hip joint is increased by metabolic and hormonal disorders, smoking, unhealthy eating habits, and obesity.Endocrine and metabolic disorders play a significant role in the prevalence of hip osteoarthritis, especially in women. This is related to the influence of certain hormones, especially estrogen, on bone tissue metabolism in postmenopausal women. The correlation between obesity and the occurrence of degenerative disease of the hip joint is also observed more frequently in women than in men, and this can have both a direct and indirect impact on the evolution of degenerative changes in the hip joints.
A direct impact is associated with an increased load to which the hip joints are exposed, which can lead to mechanical damage. The indirect effects of obesity on the degenerative disease of the hip joints are, on the other hand, related to the harmful effects of metabolic changes on the conditions of the structures that form the joint (mainly cartilage). Due to hypercholesterolemia, which usually occurs with obesity, the composition of synovial fluid may be subject to change, and nutrition disorders may occur in the subchondral bone layer. Both obesity and overweight, as well as the onset of diabetes, have a considerable impact on the faster development of hip osteoarthritis.
Age is an even more important risk factor. In younger people (under 30-35 years), this disease is very rare. Later, at the age of 40-45, it affects approximately 2-3% of the population, but after the age of 65 the number of people with osteoarthritis of the hip explodes: at the age of 45-65, almost a third (30%) can suffer of this condition, and at the age of 65-70 the probability of degenerative osteoarthritis increases up to 70-75% or more!
In other words, most seniors have some signs of degenerative joint disease and probably they may be hip osteoarthritis.
Symptoms of hip osteoarthritis
The symptoms of hip osteoarthritis are pronounced, so diagnosis is easy. However, you must remember that the symptoms of hip osteoarthritis depend on the degree of the disease. The major signs of the disease include:- Joint pain, which does not pass even during rest, and nocturnal pain. The pain intensifies even with little physical exertion and extends to the groin, knees, tibia, and hip.
- The constant tension of the pelvic muscles or hip muscles.
- Stiffness and significant limitation of joint mobility.
- Limping as you walk.
- Cracking in the joints.
- Over time, the patient's limb becomes shorter, and the muscles atrophy.
- Deformation of the joint.
The symptoms of bilateral or symmetrical hip osteoarthritis are the same but are present at both extremities. A specific feature is that the pathological process extends to the lumbosacral spine. Minor movements lead to deformity of the spine and, over time, the prominence of the intervertebral discs and the bending of the spine appear.
Grade 1 hip osteoarthritis it is characterized by the appearance of periodic pain sensations in patients, this being observed after certain forms of physical activity (running, walking, etc.). Predominantly, the location of the pain is concentrated in the hip joint, but it is not excluded that it occurs in the knee joint or in the thigh. Usually, rest promotes the disappearance of pain. There are no restrictions on movements at this stage, there are no gait abnormalities, there are also no changes in muscle strength. The femur is almost unchanged. There is an uneven narrowing of the joint gap.
Grade 3 hip osteoarthritis is characterized by a persistent manifestation of pain, not only during the day but also at night. There are pronounced difficulties in walking, you need support and the use of a cane. In addition, there is atrophy of the muscles of the lower leg, thigh, and buttocks. Due to the weakness of the femoral muscles, pelvic ablation occurs in the frontal plane, while the limb is shortened on the affected side. To compensate for the actual shortening, the patient must tilt the torso as he walks, and the movement of the center of gravity leads to a sharp increase in the load, which, in one way or another, falls on the affected joint.
Consequently, all these processes minimize the mobility of the affected joint due to the practical insertion of the femoral head into the acetabulum. Due to the fact that there is almost no cartilage tissue at this stage, it can be argued that the joint is not practically rehabilitated. And even if in any way it would be possible to restore the affected cartilage tissue, due to the more advanced deformation process, which is already relevant for the femoral head, the proper functioning of the joint is impossible in any case.

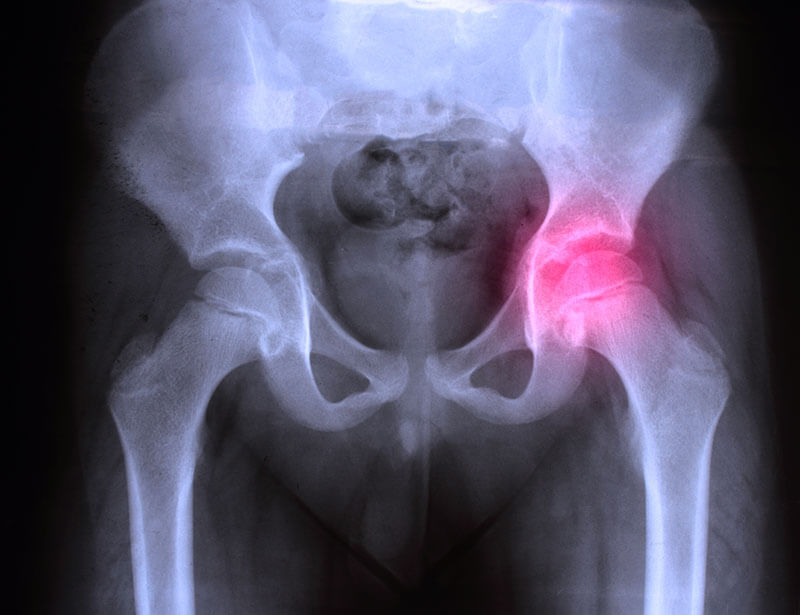
Diagnosis of hip osteoarthritis
Coxarthrosis can be diagnosed by a practicing doctor only with the help of x-rays. The examination helps to define the degree of development of the disease and its etiology.The first thing to keep in mind is the doctor's qualification: it is important for diagnosing diseases. Quite often, a specialist develops the treatment plan for the spine, forgetting to examine the hip joints and thus wasting precious time.
Currently, the following diagnostic methods are used:
- X-ray examination. This allows you to visualize the condition of the hips and highlight the symptoms.
- Ultrasound examination. This examination is necessary to define the stage of the disease and to locate the degenerative-dystrophic source.
- Computed tomography or magnetic resonance imaging. Most often, MRI is preferred due to the absence of X-rays and detailed visualization. The device allows scanning in layers, finding out the stage of the disease, and discovering it in the early stages of development.
Patients need to understand that hip osteoarthritis is a progressive disease. Even if it is revealed in the early stages and treated with medication, there is no 100% guarantee that it will be completely eliminated. In most cases, the disease can be stopped, but practice shows that the mechanism of its development restarts within 5-10 years.
Possible complications of hip osteoarthritis
Most often, hip osteoarthritis is complicated by the destruction of bone tissue. Other complications of hip osteoarthritis include aseptic necrosis of the femoral head, protrusion of the acetabulum, destruction of cysts in the acetabular region. In some cases, the rapid progression of hip osteoarthritis can lead to an unusual reaction - pronounced destruction of bone tissue and a wide joint. This variant of hip osteoarthritis is called "analgesic hip joint" because it is associated with the administration of pain medications. However, it can also develop in patients who do not take any or too few painkillers.Coxarthrosis may occur again on the background of contralateral or ipsilateral gonarthrosis. Among the complications of periarticular structures, trochanteric bursitis most often develops.

Treatment of hip osteoarthritis
In stage I of the disease, doctors prefer conservative treatment and apply various drugs and products (nonsteroidal anti-inflammatory drugs, neuromuscular relaxants, cartilage protectors and other drugs). Non-steroidal anti-inflammatory drugs are pain prevention agents for hip osteoarthritis and reduce swelling and inflammation of the joints, relieving pain.Muscle relaxants also reduce muscle spasms, stimulate blood flow, and cartilage protectors help restore damaged cartilage tissue. These medicines can be used as pills and injections, depending on the degree of pain and the doctor's prescriptions.
Physical therapeutic methods are also important in the treatment of hip osteoarthritis (laser therapy, baths, acupuncture, mud treatment, massage, and gymnastics). A specialist must ascertain very precisely the exercises in order not to traumatize the damaged joint.
Arthroscopic debridement is used in the first and second stages of the disease - it is a surgery during which small destroyed cartilage particles are removed. It reduces pain and constraints in the joint. Juxtarticular osteotomy is a surgery in which the hip bone is cut in certain places and is reintroduced at a certain angle which allows the development of hip osteoarthritis to be slowed down.
Drug treatment for hip osteoarthritis
Drug therapy is based on symptomatic treatment: elimination of pain, swelling, and inflammation, normalization of blood circulation, nutrition of cartilaginous tissue.Non-steroidal anti-inflammatory drugs (diclofenac, Ketoprofen, Indomethacin) are used to combat the disease in the acute form of the inflammatory process. The disadvantage of these drugs is addiction, and their side effects affect the internal organs. The mildest drug today is Movalis, it has the fewest side effects and does not cause rapid addiction. It is not recommended to receive more anti-inflammatory agents. If the prescribed medicine is not effective, it is necessary to change the dose or take other means.
Vasoconstrictor therapy will help relax the vascular smooth muscles and widen the distance between them to ensure normal blood circulation. Such drugs relieve spasms of blood vessels.
The category of muscle relaxant drugs (Midocalm) is used to relieve painful muscle spasms, to normalize blood flow and flow. But they must be administered for a short period to avoid side effects.
Chondroprotective drugs are the most effective. Their task is to regenerate cartilage structures. The systematic use of such drugs is an excellent prevention of hip osteoarthritis and its treatment from the beginning. Regular use stops the disease in its initial stages.
Hormonal intramuscular or intra-articular drugs (hydrocortisone) are used if there is no inflammation. You can use them every two weeks.
Surgery
When the disease reaches the third stage, the joint tissues hardly react to restoration therapy. The patient suffers from permanent pain, and the ability to move is almost lost. At this stage, there is no point in using cartilaginous protectors for treatment - the disease can be cured by conservative methods. In such cases, the doctor may decide to treat hip osteoarthritis with surgery.Why can't surgery be avoided in 99% of cases? Usually, the pain occurs when the joint already has the second stage of destruction. In other words, the main feature of hip osteoarthritis is that it is not usually diagnosed in the early stages because the patient has no symptoms.
Surgical treatment of hip osteoarthritis involves performing one of the following operations:
- Arthroplasty - modeling of joint surfaces. To perform this operation, a doctor must make a replica of the cartilaginous tissue. It can be made either of synthetic materials or with the patient's own tissues.
- Endoprosthesis - this operation is done in the case of bilateral osteoarthritis of the hip joint. During the operation, the hip joint is completely replaced. This surgery does not involve cutting the muscles, so the restoration after is relatively fast.
- Osteotomy - an operation that involves cutting bones, removing deformities, and joining them in the most advantageous way. In some cases, partial joint movement may be preserved.
- Arthrodesis - the operation in which the articular surfaces are rigidly interconnected by means of plates and screws. In this way, the movement of the joint is reduced or totally eliminated. It is performed to restore at least the support function of the legs and joints. This method is used in cases where all other options are impossible, for example, if there are no contraindications or when the hip joint is severely deformed.
Before the operation, the patient should go through a detailed examination: blood test, an x-ray of the hip affected by hip osteoarthritis, urine test, and electrocardiogram.
In addition, the patient should be examined by a dentist and, if necessary, go through dental treatment. Some dental problems are associated with a high risk of developing an infection after surgery.
Because this operation is usually performed under general anesthesia, the patient is not allowed to drink and eat in the morning before surgery.
Hip prosthesis
For osteoarthritis of the hip joint, both the ball and the sac of the joint must be replaced with an artificial joint, known as total hip replacement.The continuous improvement of both surgical techniques and the quality of implants since 1960 makes this procedure one of the most common and most successful routine operations in orthopedic surgery, with a total of approximately 400,000 operations per year in Europe as a whole.
The prosthesis is modeled on the real human joint. The preoperative planning scheme is used to specify the size of the model and the fixation of the prosthesis, respecting the individual requirements (age, sex, bone shape, bodyweight, etc.).
Stages in the surgical implantation of the artificial hip joint
In implantation, three different fixing techniques are used:
- Fixing the stent without cement
- Fixation of the cemented endoprosthesis
- Fixation of the hybrid stent
Alternatively, the base in a cemented prosthesis is made of polyethylene. For this traditional approach, implants with many years of proven reliability are available.
For cemented prostheses and normal wound healing, the treated foot can soon carry the maximum weight. Partially cemented and cementless implanted prostheses can be exposed in the first two weeks to 10-20 kg loads only; after that, progress to full weight is possible.

Alternative treatments to relieve the symptoms of hip osteoarthritis
Although few dare to talk to their doctor about this, many patients resort to alternative treatments to relieve the symptoms of hip osteoarthritis, especially pain. The term "alternative treatment" is used with caution because some drugs called "alternatives" cause side effects.The various alternative therapies used for hip osteoarthritis include homeopathy, herbal medicine, oligotherapy, acupuncture, mesotherapy, osteopathy, and chiropractic.
Balneotherapy
Balneotherapy is a type of water therapy that aims to reduce pain and improve daily functioning. Balneotherapy is often performed in centers with thermal baths or sea-water baths. Balneotherapy or spa therapy is an old and popular therapy. This involves spending time in an indoor pool filled with mineral water at a temperature between 31 and 34 degrees Celsius. Different types of mineral water can be used in this therapy.The time spent in a mineral bath, compared to the lack of treatment, can lessen the pain and improve the quality of life. The time spent in both the sulfur bath and a bath with water from the Dead Sea, compared to the lack of treatment, can relieve the pain one month after treatment.
Massage
People with hip osteoarthritis who suffer from chronic symptoms may consider regular use of massage therapy, even daily use of self-massage to help manage pain and stiffness and to promote better sleep which can relieve pain in muscles and joints.Massage therapy is an ancient form of pain and stress relief practiced by most cultures around the world. These techniques can involve not only the physical manipulation of body tissues but also relaxation techniques. Massage may involve the use of heat and cold packs on the skin, or the use of oil or lotion to ease the sliding of hands or tools on the skin. An experienced technician who works specifically to improve blood circulation, spasms, and swelling must perform the massage. Massage offers a positive result in combination with therapy.

Physical therapy
Movement in hip osteoarthritis is one of the important components of treatment. To know what exercises and movements you need to do to relieve pain and stop the progression of the disease, it is necessary to work with a physical therapist. Exercise is selected according to the degree of development of the disease, they should not put a heavy weight on the affected joint, and should aim at strengthening muscles.Before moving directly to physical therapy exercises, you need to consider some recommendations for their correct application:
- the exercises must be mostly static, the movements must not be too energetic, with excessive amplitude, and not cause pain;
- the muscles of the thigh and hip should be massaged before the exercises begin and after their completion;
- completely forbidden: excessive physical exercises, deep and fast knee bends, pelvic balancing;
- Physical exercises for the hip can be performed in a warm bath which promotes relaxation and release of muscle stress.
Phytotherapy
Herbal medicine or herbal medicine is a treatment that uses plants with therapeutic properties (or, more precisely, the "active part" of these plants, the richest part of the active ingredients). Once the plants are collected, different methods perform the extraction. The extracts can then be administered in capsules, teas, pure extracts, etc.The herbal medicine uses plant extracts obtained using the same preparation techniques as those used to obtain the compounds that provide the basis for homeopathic dilutions. The difference is the origin of the extracts used in homeopathy, which are of vegetable origin, but also animal and mineral.
As with homeopathy, these remedies claim to have properties that relieve hip pain, but their effectiveness is not scientifically proven, and these remedies do not replace conventional drugs.
Acupuncture
Acupuncture, a therapeutic method that is part of Chinese medicine, was born several centuries before Christ. The acupuncture technique is based on placing metal needles on certain points of the human body along the meridians, to relieve pain or symptoms of the disease.The analgesic and relaxing effect helps some patients who have hip osteoarthritis. However, no scientific evidence has been provided to demonstrate the effectiveness of acupuncture in relieving hip pain. The main complication is local irritation if the skin is sensitive.
Natural treatments
Most patients who experience this disease prefer to eliminate the discomfort through drug therapy, ie to apply the popular method of healing. Independently at home, you can make tinctures, decoctions, and effective mixtures. Here are some examples:- Lilac tincture.
- Valerian tincture.
- The mixture of parsley root, willow bark, burdock, birch leaves, and linden flower.
To get a positive dynamic, there must be a diet. Vitamins must be consumed to restore the body. Special attention is paid to plant foods. It is recommended to eat more vegetables and fruits. These will restore the damaged joint and thus ease the symptoms of hip osteoarthritis.

Prevention of hip osteoarthritis
Although you can't prevent all hip problems, many of the same measures used to treat hip problems can reduce your risk of hip osteoarthritis or worsening it. Weight loss, for example, can help prevent hip osteoarthritis from progressing, and proper exercise can help reduce the risk of pain and injury.Accident prevention measures and their careful treatment when they happen can avoid more serious problems and certain painful diseases, such as coxarthrosis.
The following tips can help you:
- Lie down and warm up before any workout.
- Don't exaggerate. If you suffer from pain when exercising, stop, and relax.
- Wear appropriate shoes.
- Avoid running on hard surfaces, such as asphalt and concrete, when possible.
One of the most popular remedies for joint health is glucosamine, a common dietary supplement derived from shells (mussels). Glucosamine is often combined with chondroitin, a substance found naturally in cartilage, but is made from animal sources, such as bovine cartilage. Laboratory studies have shown that it nourishes cells - the theory is that it helps preserve cartilage in the body. Glucosamine is also thought to act as an anti-inflammatory. Vegetarian varieties are available for people allergic to shellfish.
Do not ignore the early signs of any condition. The faster you get to the doctor, exponentially the chances of healing or controlling the condition increase.
IN CASE YOU HAVEN'T ALREADY HEARD ABOUT US
Centrokinetic is the place where you will find clear answers and solutions for your motricity problems. The clinic is dedicated to osteoarticular diseases and is divided into the following specialized departments:
- Orthopedics , a department composed of an extremely experienced team of orthopedic doctors, led by Dr. Andrei Ioan Bogdan, primary care physician in orthopedics-traumatology, with surgical activity at Medlife Orthopedic Hospital, specialized in sports traumatology and ankle and foot surgery.
- Pediatric orthopedics , where children's sports conditions are treated (ligament and meniscus injuries), spinal deformities (scoliosis, kyphosis, hyperlordosis) and those of the feet (hallux valgus, hallux rigidus, equine larynx, flat valgus, hollow foot).
- Neurology , which has an ultra-performing department, where consultations, electroencephalograms (EEG) and electromyography (EMG) are performed.
- Medical recovery for adults and children , department specialized in the recovery of performance athletes, in spinal disorders, in the recovery of children with neurological and traumatic diseases. Our experience is extremely rich, treating over 5000 performance athletes.
- Medical imaging , the clinic being equipped with ultrasound and MRI, high-performance devices dedicated to musculoskeletal disorders, and complemented by an experienced team of radiologists: Dr. Sorin Ghiea and Dr. Cosmin Pantu, specialized in musculoskeletal imaging.
Find the latest news by following the Facebook and YouTube accounts of the Centrokinetic clinic.
SUCCESSFUL RECOVERY STORIES

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT