See details
READ MORE
Osteoarthritis, a complex condition
Osteoarthritis is a degenerative disease that cannot be cured, but there are many ways we can improve it. To prevent aggravation, you must keep in mind some strict rules that will help you in the long run.Next, we will tell you everything about osteoarthritis, from the main causes and factors to the diagnosis, types of treatment, and prevention tips, to avoid common mistakes in advance.
Centrokinetic welcomes patients with a complete rheumatology department, a medical branch that deals with the diagnosis, treatment, and recovery of patients with non-surgical musculoskeletal disorders. These conditions are usually painful, acute, or, most often, chronic, preventing the proper functioning of the musculoskeletal system. They are generally called rheumatism or rheumatic and musculoskeletal diseases.
Most of the time, the evaluation of the patient is complex, multidisciplinary, considering the systemic, generalized character of most rheumatic diseases. That's why Centrokinetic has experienced doctors, Dr. Alizzi Khalid being our specialist in rheumatology.
What is osteoarthritis
Osteoarthritis is a degenerative disease of any joint. This disease is usually caused by chronic wear of the cartilage in the joint which eventually leads to the complete removal of the cartilage. Osteoarthritis is most common in the joints of the knees, hips, hands, and spine. However, it can affect any joint.
Causes and risk factors for osteoarthritis
The main cause of osteoarthritis is the mechanical stress on the articular surface of the cartilage, and the cartilaginous tissue cannot resist this stress. Therefore, osteoarthritis often develops in people who work hard or in those who use their joints excessively through repeated movements and, of course, in athletes. Osteoarthritis occurs when the intra-articular cartilage is damaged. Cartilage is a firm, slippery tissue that allows joint movements almost without friction. In osteoarthritis, the slippery surface becomes hard. Finally, if this cartilage is completely damaged, bone-to-bone contact occurs.
Factors that may increase the risk of osteoarthritis are:
- Age - With age, the risk of osteoarthritis increases.
- Sex - Women are more likely to develop osteoarthritis, although it has not yet been discovered why.
- Obesity - Carrying extra body weight contributes to the development of osteoarthritis in many ways, and the heavier the weight, the greater the risk of developing it. Obesity causes an increase in effort for the joints, such as the hips and knees. In addition, fatty tissue produces proteins that can cause harmful inflammation in and around the joints.
- Joint Injuries - Accidents, such as those that occur after playing a sport, or any other type of accident, can increase the risk of developing osteoarthritis. Even injuries that occurred many years ago and are apparently cured can increase the risk of developing osteoarthritis.
- Certain Occupations - If your occupation includes repetitive stress on a joint, that joint may eventually develop osteoarthritis.
- Genetics - Some people inherit a tendency to develop osteoarthritis.
- Bone deformities - Some people are born with malformed joints or defective cartilage, which increases the risk of developing osteoarthritis.
![]()
Symptoms of osteoarthritis
Although osteoarthritis can occur in any joint, the most affected are the joints of the hands, knees, hips, and spine, either in the neck or lower back. The different features of the disease may depend on the specific joints affected.
For information on the joints most often affected by osteoarthritis, see the following descriptions:
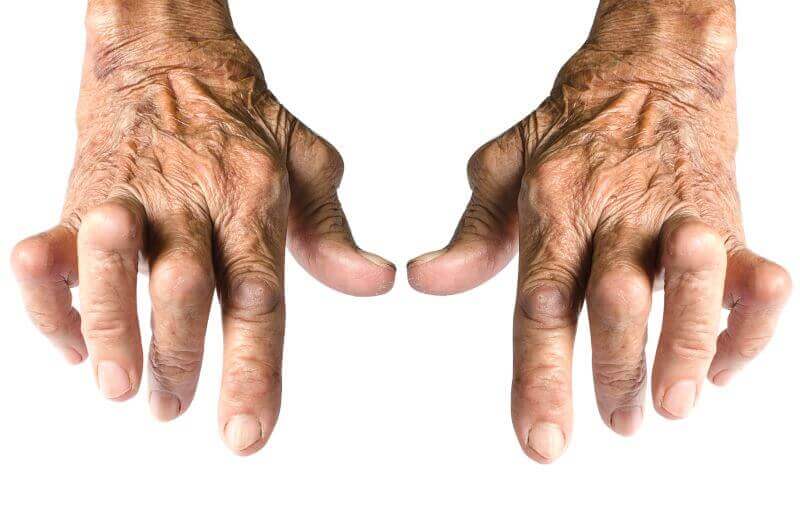
- Hands - Osteoarthritis of the hands seems to have certain hereditary characteristics. If your mother or grandfather has or has had osteoarthritis of your hands, you are at high risk of developing osteoarthritis of your wrists. Women are more likely than men to have osteoarthritis in their hands. For most women, it develops after menopause.
- Knees - The joints most commonly affected by osteoarthritis are those of the knees. Symptoms include stiffness, swelling, and pain, which makes it difficult for the person to walk. Osteoarthritis of the knee can lead to disability.
- Hips - As with osteoarthritis of the knee, the symptoms of hip osteoarthritis are similar. But sometimes the pain is felt in the groin, inner thigh, buttocks, or even the knees. Osteoarthritis of the hip can limit movement and bending, making daily activities, such as dressing or wearing shoes, a real challenge.
- Spine - Osteoarthritis of the spine can occur in the form of stiffness and pain in the neck or back. Sometimes, changes associated with osteoarthritis of the spine can cause pressure on the nerves, leading to weakness, tingling, or numbness of the arms and legs. In severe cases, it can even affect the function of the bladder or intestine.
![]()
Types of osteoarthritis
There are 6 different types of osteoarthritis: cervical, facet joint, hip osteoarthritis, lumbar, knee, and acromioclavicular. Osteoarthritis can affect any joint in the body, and the risk of developing a certain type of osteoarthritis increases with age. Cervical osteoarthritis
Cervical osteoarthritis affects the cervical vertebrae. Cervical osteoarthritis is often related to age and triggered by stress and wear and tear. It is associated with chronic neck problems. Symptoms of cervical osteoarthritis include:
- stiffness and pain in the neck
- muscle spasms
- tension-type headaches
- muscle stiffness
Osteoarthritis of the articular facets
Facets are joints between the vertebrae that extend along the spinal cord. The causes of facet arthritis are wear and tear, anxiety over the years, and stress. The wrong position can also contribute to this type of osteoarthritis because it focuses on these joints. This type of osteoarthritis is more common among the elderly and can cause back pain, especially in an upright position. The location of the pain can help determine the affected facets.Coxarthrosis
Coxarthrosis, also called osteoarthritis of the hip joint, is very common in older people. The hip joint is a ball and socket joint and is one of the strongest in the body, it supports a lot of weight and stress. Coxarthrosis is caused by wear and tear, so it is found more often in the elderly and athletes, but can also be found in people who are overweight.
The symptoms of this type of osteoarthritis are hip pain, which worsens when you walk more or stay too long in a certain position, is manifested by a crack in the joint when walking, and a limitation in the foot's movement.

Gonarthrosis or osteoarthritis of the knee
The most common reason for knee joint disorders is cartilage wear (osteoarthritis), caused mainly by misalignment of the axes of the foot. Also, gonarthrosis occurs as a result of injuries, rheumatic, and metabolic disorders, as well as deformities.Loss of cartilage leads to increased stiffness and joint deformity. There is pain, first associated with the initial movement after a longer period of inactivity and stress, later at night and at rest, which leads to a limitation of walking and ultimately to a reduced quality of life.
Lumbar Osteoarthritis
Lumbar osteoarthritis affects the lower back, the area of the body that supports the most weight, and pressure. In principle, it is caused by years of poor posture and abdominal obesity. Symptoms include pain in the lower back, which worsens when standing upright, and loss of flexibility.
Acromioclavicular osteoarthritis
The acromioclavicular joint is located in the shoulder. This osteoarthritis is caused by normal wear and tear, but can also develop because of a shoulder injury. We commonly see this type of osteoarthritis when lifting weights. Symptoms include sensitivity, pain, limited mobility, and flexibility, as well as depressing sound.

Diagnosis of osteoarthritis
To diagnose osteoarthritis, your doctor will collect information about your personal and family medical history. Dr. Alizzi Khalid will perform a physical examination and after that, together with the present symptoms, the doctor can make a diagnosis.Description of symptoms:
- Details of when and how the pain or other symptoms appeared.
- Details about other medical problems that exist.
- Location of pain, stiffness, or other symptoms.
- How symptoms affect daily activity.
- List of current drugs.
During the physical examination, the doctor will analyze the joints and test their range of motion to see how well the movement is doing in the problem area. He will look for painful or swollen areas, and signs of joint damage. The doctor will examine the position and alignment of the neck and spine.

Complications of osteoarthritis
Most people believe that osteoarthritis is a problem that becomes significant enough to affect daily activities. Sometimes there are more serious complications, such as:- Rapid and complete destruction of cartilage resulting in free tissue in the joint.
- Osteonecrosis, also called "bone death".
- Stress fractures, which are cracks in the bone that gradually evolve in response to injury or repeated stress.
- Bleeding inside the joint.
- Infection in the joint.
- Damage or rupture of tendons and ligaments around the joint, leading to loss of stability.
- Compressed nerves, a complication that can occur in arthritis of the spine.
Treatment of osteoarthritis
Currently, the underlying process of osteoarthritis cannot be reversed, but symptoms can usually be managed effectively with lifestyle changes, physical therapies, medications, and surgery. Gaining healthy weight is usually the most important step in treating osteoarthritis.The objectives of osteoarthritis treatments
The objectives of osteoarthritis treatments are: to alleviate the pain caused by it, to improve the mobility of the joints, and to reduce the rate of its aggravation.
Relieving the pain caused by osteoarthritis
Warm therapies, such as the use of bath medicinal oils and gels that contain essential oils, can give some relief to the pain. Other therapies, such as injections of cortisone or lubricant into the joints, and even joint replacement, are reserved for severe cases. If your work or hobbies have caused osteoarthritis, our medical team can help you with tips in avoiding additional damage. Plantar supports can help reduce stress and pressure on affected joints.

Improving joint mobility
Physiotherapy can help you reduce joint pain and improve your mobility by incorporating a variety of techniques into a treatment program: including manual therapy, stretching, and strengthening exercises.Reducing the rate of osteoarthritis
The damage caused by osteoarthritis is usually progressive, and the longer you wait for treatment, the more damage can occur to the joint. Treatments with natural supplements can delay the development of osteoarthritis and can help the patient reduce pain.
Drug Treatment
Osteoarthritis medications are available as pills, syrups, creams, lotions, or are injected.Steroids are powerful anti-inflammatory drugs that can treat many forms of osteoarthritis. Although effective, steroids can have side effects, especially when taken as pills and used for a long time. Often, our medical team tries to avoid these problems by injecting the steroid into the affected joint or by trying other drugs in combination to keep the steroid dose as low as possible.
Hyaluronic acid injections
There are several types of injections of hyaluronic acid, also called viscosity supplements, which are used by Dr. Alizzi Khalid for the treatment of osteoarthritis of the knee. They are injected directly into the joint. Some studies have shown a benefit in reducing pain for periods of up to six months.Natural treatment of osteoarthritis
Natural supplements can help treat osteoarthritis or reduce its rate of exacerbation. S-Adenosyl-Methionine (SAM-e) acts as an analgesic and has anti-inflammatory properties. It can stimulate cartilage growth and also affects neurotransmitters such as serotonin, which reduces the perception of pain. Studies have shown that it relieves the symptoms of osteoarthritis as effectively as nonsteroidal anti-inflammatory drugs, with fewer side effects and prolonged benefits.The active ingredients in Indian Incense (Boswellia Serrata) have anti-inflammatory and analgesic properties. Incense can also help prevent cartilage loss and inhibit the autoimmune process. The extract, also known as Loxin 5, can significantly improve pain and slow the development of cartilage damage.

Surgery for osteoarthritis
Joint replacement is usually very effective in relieving pain. The degree to which movement can be improved will depend on how severe the osteoarthritis is and how strong the muscles around the joints are. Hip and knee replacement are now very common procedures. Although most people undergoing these joint replacements are patients over the age of 65, the improvements in design and materials used for implants also help younger people to accept the operation more easily. Replacement of the hip or knee should take about 15-20 years, depending on wear, after which a revision surgery may be considered.Arthroscopy
Arthroscopy is a process that allows the doctor to see directly into the joint with the help of an instrument called an arthroscope. This is a very thin tube, which has a camera attached and allows the surgeon to see on the screen what is happening in the joint. Arthroscopic surgery can be used to find out what kind of osteoarthritis exists, and how many lesions are present. The surgeon can also perform many other procedures, such as biopsy, cutting a free piece of tissue that causes pain, repairing torn cartilage, or smoothing a joint if the surface has become rough.Extensive surgery, such as synovectomy or ligament reconstruction, is also performed with an arthroscope. The advantage of arthroscopic surgery is that it does not require total anesthesia, nor cut tissue as in standard surgery. A person can recover much faster and can start walking faster. The procedure is most often done on the knee or shoulder, but lately, it has been used on other joints, such as the elbow, wrist, and ankle.

Physiotherapeutic procedures to treat osteoarthritis
Physical therapy aims to reduce pain by restoring joint movement and improving muscle function. After a thorough evaluation, your therapist will determine what exactly causes the discomfort and stiffness, and together you will develop a program that will help you regain joint movement.Physical therapy for osteoarthritis includes:
- joint mobilization, pulley therapy
- tractions, which help increase joint mobility
- restoring the stability obtained through exercises
- coordination and balance exercises
- muscle relaxation through massage
Procedures and exercises for restoring posture
Exercises are very important in restoring normal movement. Patients with osteoarthritis tend to limit movement in the affected joint, and the muscle in the area is very little stressed. A special exercise program, recommended by the therapist, will help the patient regain his posture and get rid of the pain in the joints and muscles.Certain disciplines have proven to be effective, and one of them is a Chinese technique. Tai Chi - a Chinese martial art, is often used to reduce stress and tension, while the body moves through the functional range of motion. Participants are helped to achieve complete relaxation. The movements used in Tai Chi are simple and slow, encouraging patients to adopt a correct posture when exercising.

Procedures and exercises to improve mobility
It is difficult for a person suffering from joint pain to remain active. Regular physical activity is crucial for your overall health, but also for nourishing and strengthening muscles and, therefore, improving joint mobility. Although not at all comfortable at first, the movement reduces pain and the effects of osteoarthritis.It is important to choose a sport that is right for your problem. If you suffer from knee osteoarthritis, avoid certain sports, such as running or skiing. In the case of lumbar arthritis: cycling, golf, and tennis are not recommended.
In all cases of osteoarthritis, swimming is an excellent sport, because it requires several muscles simultaneously, without creating a direct impact on the join
Procedures and exercises to improve stability
For joints to function properly, they must be stable or mobile depending on the activity. Some joints are more stable, while others are more mobile. When approaching balance, the important joints for stability are the lumbar spine, knees, and legs. The hips and ankles are more mobile. While balance is important for anyone, balance exercises are especially indicated for seniors and those who have had joint replacement surgery. Practicing balance exercises can help reduce the risk of falling.Example of balance exercise: position on one leg
Once you have found balance on two legs, progress to balance on one. Sit on a flat surface. Raise your right foot a few inches off the ground, with your leg straight or bent and your arms at your sides. Stand in position for 30 seconds. If it is easy, try to close your eyes and stand on one leg for another 30 seconds. Change your leg and repeat.
Psychotherapy, important for encouraging the patient and increasing the effectiveness of treatments applied.
In patients with osteoarthritis, socio-psychological factors that affect the disease process, such as poor social relationships, communication disorders with the environment, unhappiness, and depression at work are common.
Psychotherapy helps and educates patients by giving them information about their condition and about physical therapy and rehabilitation options that are available to improve their quality of life.
Tips for preventing osteoarthritis
Unfortunately, there is no safe way to prevent osteoarthritis. But it can reduce the risk and delay the onset of certain types of osteoarthritis.If you have healthy joints now, do everything you can to maintain their mobility and function, to avoid the pain and disability associated with osteoarthritis. Sometimes, preventing an accident can significantly reduce the risk of osteoarthritis.
Avoiding sports injuries by wearing the right equipment, preparing, and training safely can prevent certain ligament tears that can lead to osteoarthritis in a few years. Also, maintaining optimal body weight and adopting a healthy lifestyle can significantly reduce the risk of this condition and other diseases.
Do not ignore the early signs of any condition. The faster you get to the doctor, exponentially the chances of healing or controlling the condition increase.
IN CASE YOU HAVEN'T ALREADY HEARD ABOUT US
Centrokinetic is the place where you will find clear answers and solutions for your motricity problems. The clinic is dedicated to osteoarticular diseases and is divided into the following specialized departments:
- Orthopedics , a department composed of an extremely experienced team of orthopedic doctors, led by Dr. Andrei Ioan Bogdan, primary care physician in orthopedics-traumatology, with surgical activity at Medlife Orthopedic Hospital, specialized in sports traumatology and ankle and foot surgery.
- Pediatric orthopedics , where children's sports conditions are treated (ligament and meniscus injuries), spinal deformities (scoliosis, kyphosis, hyperlordosis) and those of the feet (hallux valgus, hallux rigidus, equine larynx, flat valgus, hollow foot).
- Neurology , which has an ultra-performing department, where consultations, electroencephalograms (EEG) and electromyography (EMG) are performed.
- Medical recovery for adults and children , department specialized in the recovery of performance athletes, in spinal disorders, in the recovery of children with neurological and traumatic diseases. Our experience is extremely rich, treating over 5000 performance athletes.
- Medical imaging , the clinic being equipped with ultrasound and MRI, high-performance devices dedicated to musculoskeletal disorders, and complemented by an experienced team of radiologists: Dr. Sorin Ghiea and Dr. Cosmin Pantu, specialized in musculoskeletal imaging.
Find the latest news by following the Facebook and YouTube accounts of the Centrokinetic clinic.
SUCCESSFUL RECOVERY STORIES

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT