See details
READ MORE
- Spondylosis, a condition that is becoming more common
- What is spondylosis
- Symptoms of spondylosis
- Causes of spondylosis
- Types of spondylosis
- Risk factors for spondylosis
- Diagnosis of spondylosis
- Complications of untreated spondylosis
- Treatment of spondylosis
- Procedures for treating spondylosis
- Drug treatment for spondylosis
- Natural treatments to relieve spondylosis
- Surgical treatment for spondylosis
- Methods to prevent spondylosis
Spondylosis, a condition that is becoming more common
Spondylosis is also known as spinal osteoarthritis - a fairly common condition, but it is usually not serious, although it can be quite painful. As with many other terms for describing spinal problems, spondylosis is more of a descriptive term than a clinical diagnosis. It can be translated to mean both pain and degeneration of the spine, regardless of what causes the pain or where the degeneration occurs.Spondylosis is becoming more common. Symptoms are often reported between the ages of 20 and 50. Over 80% of people over the age of 40 have spondylosis in radiographic studies. The rate at which spondylosis occurs is partially related to genetic predisposition, as well as the history of lesions.
What is spondylosis
Spondylosis is an aging phenomenon. With age, worn bones and ligaments in the spine lead to bone spurs (osteoarthritis). Also, the intervertebral discs degenerate and weaken, which can lead to disc herniations and bulging discs. It can affect any region of the spine: the cervical area (neck), the thoracic area (upper back, middle back), and the lumbar area.Most patients with spondylosis do not require surgery on the spine. However, aging is an individual process. Some people will feel the effects (especially pain) of the aging spine earlier, and others may not have pain in the spine at all. It all depends on how the parts of the spine change, and whether these changes affect the spinal cord or spinal nerves.
Symptoms of spondylosis
Symptoms depend on where the spine is affected by spondylosis. These symptoms can range from mild to severe and can become chronic. These may include:Neck (cervical area)
- The pain that appears and disappears
- Pain that spreads to the shoulders, arms, hands, or fingers
- Stiffness in the morning in the neck or shoulder, or a limited range of motion
- Numbness of the neck or shoulder
- Weakness or tingling in the neck, shoulders, arms, hands, or fingers
- Headache felt in the nape of the neck
- Loss of balance
- Difficulty swallowing (This is rare, but may occur if the spinal cord is compressed.)
- Pain in the upper and middle sections of the back
- Bending and enlarging the body triggers pain
- Stiffness in the back when getting out of bed in the morning
- Pain that appears and disappears
- Stiffness in the back in the morning
- Pain that decreases after rest or exercise
- Weakness or numbness in the lower back
- Sciatica (mild to severe pain in the foot)
- Weakness, numbness, or tingling in the back, legs, or soles
- Difficulty walking
- Intestinal or bladder disorders (this is rare, but may occur)

Causes of spondylosis
Aging is the predominant cause of spondylosis. Our bodies are subjected to a lot of stress every day and, over the years, this can change the different structures of the spine. Even before you feel the symptoms of spondylosis - pain and stiffness, for example - the joints and other structures of the spine degenerate.The main cause is aging, but the way aging affects the spine can lead to other changes and problems. Spondylosis is a cascade: an anatomical change occurs, which leads to degeneration and changes in the structures of the spine. These changes combine to cause spondylosis and its symptoms.
Degenerative disc disease
The parts of the spine that initially degenerate are the intervertebral discs. For this reason, patients with spondylosis often suffer from degenerative disc disease. The effects of these two spinal conditions are highly correlated. By degenerating, the disc will become less spongy and much thinner. A thinner disc means that the space between the vertebra above and below the disc becomes smaller, which causes an additional problem, this time in the articular facets. They help stabilize the spine, and if the disc loses its height, the way the facet joints move changes. Then, the cartilage that protects the facets begins to move away, probably causing irritation and inflammation of the spinal nerve roots.
Abnormal spinal movement
This hypermobility causes another change in the spine. It tries to stop the movement by developing small bone elements called bone spurs (osteophytes). Unfortunately, bone spurs sometimes catch nerve structures and cause pain. Bone spurs can narrow the space for the spine and nerves - this disorder is called spinal stenosis. Degenerative disc disease will not cause spinal stenosis in everyone, but it is something you should know if you have spondylosis.
The role of genetics
Your genes can also cause spondylosis. You may be prone to excessive wear on your joints and discs, so if someone in your family has or has had spondylosis, you may develop spondylosis-related back or neck pain.
Lifestyle
The way you live could lead to spondylosis. Smoking, for example, adversely affects your discs and can cause them to degenerate faster. Smoking decreases the amount of water in the discs, and water is part of what helps the discs absorb shocks. With low water content, the intervertebral discs can wear out earlier.
Types of spondylosis
The problems that spondylosis creates in the cervical and lumbar areas are the ones that most frequently affect patients' quality of life. The symptoms of spondylosis in these two areas are the most pronounced. Spondylosis can be of three types, depending on the affected bones. Cervical spondylosis - it affects the cervical vertebrae of the neck, thoracic - it affects the vertebrae that are part of the chest wall, ie the thoracic vertebrae, and lumbar spondylosis - here, the lumbar vertebrae are affected by the process of spondylosis.Cervical spondylosis
As mentioned above, this is a degeneration of the neck vertebrae. Cervical spondylosis narrows the spinal canal of the neck. This is the passage through which the spinal cord passes. This narrowing causes compression of the spinal nerves causing pain, and in many cases dysfunction. Symptoms may reflect damage to the spinal cord or nerve root. When the bone marrow is damaged or damaged, a change in position and pace of walking are often the first signs. The neck can become very painful, especially when the nerve roots are affected. Damping and weakness can develop in the arms, which is another sign of compression affecting the spinal cord.Lumbar spondylosis
Spondylosis of the lower back or lumbar region results in a pronounced, unnatural movement of the vertebrae toward each other. Despite all the upper body weight that is in this area, the degeneration of the spine described above takes place with a greater effect. The resulting common symptom is pain in the lower back, which radiates to one or both legs. Lower back pain occurs primarily due to gradually malformed vertebrae that rub against each other incorrectly. Pain, numbness, and weakness of the legs are caused by pressure on the nerves.
An MRI, performed with the patient lying on the bed, may show nothing because the condition in this area is not present in a prone position. For clarity of lumbar spondylosis, MRI should be performed when the patient is standing, leaning forward, and leaning back. This allows MRI to clearly show how the vertebrae interact, and what effect they have on the spinal canal and nerves.
Thoracic Spondylosis
A fundamental definition of thoracic spondylosis is that it is a condition that can lead to narrowing of the spinal canal in the upper and middle back, resulting in compression of the spinal cord and nerve roots. In the long run, this compression can result in damage to these structures, causing symptoms such as weakness and numbness in the upper extremities, impaired gait, and even pain in the arm.Thoracic degeneration of the spine is not as widespread as lumbar or cervical. It is predominantly caused by age-related risk factors. The spinal cord is made up of several bone segments separated by cartilage plaques that cushion the impact on the vertebrae, and the general stress on the spine. These gel-like cartilage pads are called discs, and as time passes, the body's natural changes lead to dehydration and loss of effectiveness, resulting in back pain. There is also a risk of herniated discs as the spondylosis gets worse.
Risk factors for spondylosis
Risk factors for different types of spondylosis include age, occupation, past accidents, genetic factors, smoking, body weight, etc.Risk factors for lumbar spondylosis include:
- Obesity - Patients suffering from obesity tend to overload the joints leading to spondylosis.
- Patients with a history of a fall or trauma in the past or who have suffered a hip injury, undergoing surgery on the spine, are more likely to develop lumbar spondylosis.
- Abnormal posture and sedentary lifestyle. Maintaining an improper way of sitting without the correct support of the back and having a sedentary life causes additional pressure on the muscles and ligaments of the joints that carry the weight, which leads to early degenerative changes.
- Patients with a strong genetic and familial predisposition are more likely to suffer from lumbar spondylosis.
- Age. Cervical spondylosis is a normal part of aging.
- Occupation. Jobs that involve repetitive neck movements, strange positioning.
- Injuries to the neck. Previous neck injuries appear to increase the risk of cervical spondylosis.
- Genetic factors. Some individuals in certain families will experience more of these changes over time.
- Smoking. Smoking has been associated with an increased sore neck.
- Age. Chest spondylosis is common in the elderly.
- Occupation. Work that includes chest movements, awkward body positioning, or carrying heavyweights that put pressure on the spine.
- Spinal cord injuries. Previous lesions in the area appear to extend the risk of thoracic spondylosis.
- Genetic factors. Some people may suffer from this condition, depending on genetic factors.
- Smoking. Smoking has been associated with extensive chest pain.
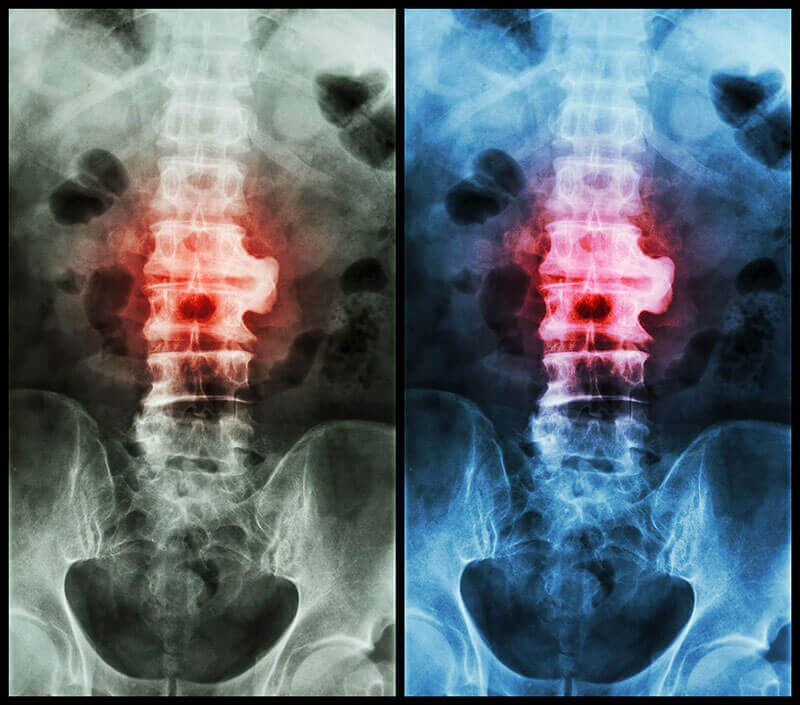
Diagnosis of spondylosis
The diagnosis of spondylosis is made by specific scans, such as MRI scans or CT scans of the spine. These scans will show a narrowing of the joint spaces between the vertebral bodies, thickening of the intervertebral discs, and highlighting the degeneration of both the discs and the vertebrae.A simple x-ray shows small protrusions known as vertebral osteophytes. The presence of osteophytes indicates osteoarthritis. These findings are quite typical and, combined with clinical history, may make it possible to diagnose spondylosis.
Physical and neurological examinations
The specialist will perform physical and neurological examinations. In the physical exam, the doctor will observe the posture, the range of motion (how well and how far you can move certain joints), and the physical condition, observing any movement that causes pain. The doctor will palpate the spine, note the curvature and alignment, and try to find where there are muscle spasms and areas of sensitivity.
During the neurological examination, the specialist will test the reflexes, muscle strength, other nerve changes, and the pain that spreads (if the pain moves from the back to other parts of the body). This evaluation also checks for other symptoms, such as numbness, tingling, bowel or bladder problems. Neurological examination is especially important in spondylosis because the condition can affect the nerves or even the spinal cord.
Complications of untreated spondylosis
LasaLeft untreated, spondylosis can have a profound effect on daily life and can lead to complications such as:- Spondylolisthesis, a condition in which the anterior slip of a vertebral body occurs compared to the rest of the vertebrae
- Limited mobility and inactivity
- Weight gain due to inactivity
- Loss of bone density
- Loss of muscle strength
- Loss of flexibility
- Permanent nerve damage
- Chronic back pain
- Numbness, tingling, or weakness in the legs
- Nerve compression that causes bowel or bladder problems
People who experience long-term pain may have difficulty concentrating, or may be unable to perform daily or professional activities.
Emotional effects
Continuous pain can lead to depression and sleep disorders. And these factors together contribute to a vicious cycle. The combination of chronic pain and depression leads to greater disability. Also, lack of sleep exacerbates the pain, and greater pain leads to the inability to sleep. Lack of sleep also contributes to depression.
Changes in the brain
Some recent studies using brain imaging have found structural changes in the brains of people with chronic back pain. There is also evidence that chronic pain leads to changes in the nerves in the spinal cord. These findings could explain why about 20% of people with back pain continue to suffer from pain even after treating the condition.
Treatment of spondylosis
Depending on which part of the spine is affected by spondylosis, treatments may differ in effectiveness and simplicity. For example, cervical spondylosis can be effectively treated with exercise and the application of a cervical collar. Patients with lumbar spondylosis may need transcutaneous electrical nerve stimulation, heat application, exercise, and painkillers to get rid of symptoms.In rare cases, patients may undergo some surgery to get complete relief from the symptoms of spondylosis. î
Most often, uncomplicated cases of thoracic spondylosis can be successfully managed using conservative therapy or non-surgical options. These treatments for thoracic spondylosis include:
- Cortisone injections
- Prescriptions for muscle relaxation
- Narcotic drugs
- Over-the-counter medications for pain or inflammation
- Heat/ice application
- Tractions
- Electrical stimulation
- Exercises
- Behavior modification
![]()
Procedures for treating spondylosis
The primary treatment for spondylosis is always conservative. The goal of conservative treatment is to reduce pain. Conservative treatment options include:
Rest: The patient should get adequate rest and avoid strenuous exercise until symptoms subside.
Medications: Non-steroidal anti-inflammatory drugs may be prescribed to reduce pain and inflammation. If nonsteroidal anti-inflammatory drugs do not provide relief, injections of epidural steroids may be given into the spine to reduce pain, numbness, and tingling in the legs.
Physical therapy: An exercise program helps strengthen the abdominal and back muscles, improves flexibility, and increases the range of motion of the lower back.
Use of prostheses: in severe cases of spondylolysis, a brace or support can be used to stabilize the lower back.
Therapy
A physical therapist can teach you exercises that help stretch and strengthen your neck and shoulder muscles. Some people with cervical spondylosis benefit from the use of traction, which can help ensure more space in the spine if the nerve roots are pinched.
Acupuncture
Your doctor may recommend that you try acupuncture to reduce pain. Acupuncture is best performed by an acupuncture specialist.
Physical therapy
If this condition has already occurred and has been medically identified, your doctor may recommend a period of physical therapy. The progression and severity of the symptoms will determine if it is necessary to stay in a clinic or hospital, or in an outpatient clinic where you can come and go daily.The goals of physical therapy in spondylosis are to rebuild muscle mass and increase muscle endurance, help the patient adapt to effort, maintain and increase joint mobility, improve muscle degeneration, coordination, control and balance, and correct posture and body alignment.
![]()
Physiotherapy
Physiotherapy, when used in combination with pain-relieving medications, can provide exceptional results through exercises that improve the strength and range of motion of the vertebrae. Physiotherapy helps minimize symptoms and can be done at home. Several forms of physical therapy aim to relieve symptoms. These include:
Hydrotherapy: Using the effects of water to relieve pressure and pain, hydrotherapy can treat a variety of disorders related to bone and joint pain. This differs from swimming because it involves exercises that you do in hot water, usually at a temperature between 32 C and 36 C. A trained physiotherapist usually demonstrates how to do the exercises in water, making necessary adjustments for patients. individual.
Tape application: This is a technique used to prevent or rehabilitate an injury. Physiotherapists are specially trained to effectively apply the tape to the skin to keep specific muscles or bones stable.
The benefits of using this form of physiotherapy include:
- Accident prevention
- Quick return to sports or work
- Protection of damaged soft tissues, such as ligaments or tendons
- Encouraging normal movement
- Pain reduction
- Reducing the risk of injury
- Improved joint stability
- Reduction of swelling
Balneotherapy
A therapist can use a gentle massage to gradually relax the muscles. It can use circulatory massage, transverse and longitudinal friction, trigger points, and other light to medium pressure techniques to relax your muscles and increase your range of motion in all directions. The goal is to minimize the progression of spondylosis and control pain. Massage is effective because it can balance and relax the muscles that support the spine.
As the therapist uses specialized hands or tools to massage, circulation is stimulated. Blood flow provides oxygen and nutrients and is essential to help muscles eliminate waste products, such as lactic acid, that can collect spasms that cause pain.
Therapeutic Laser Procedures
The concept that light energy from a laser can reduce pain and inflammation, accelerate healing of damaged tissue, relax muscles, and stimulate nerve regeneration seems to be a myth. Science, however, tells us that these effects occur, and helps patients suffering from spondylosis and beyond.
The best results will be obtained with a laser that has 30 watts of power or more. A 10-minute treatment with a 30-watt laser will produce 18,000 joules, which provides a significant pain-relieving, anti-inflammatory, and healing effect. Patients usually begin to feel better after 1 or 2 treatments, although 5 or more may be needed to resolve the problem. The more chronic and extensive the lesions, the more treatments are needed.
![]()
Ultrasound procedures
Ultrasound treatment is a treatment administered by your physical therapist. It is a supplement to primary treatment (eg, exercise). Ultrasound can help relax tight muscles that sore, warming muscles and soft tissues, which stimulates circulation that helps healing. The ultrasound equipment generates high-frequency sound waves that are transferred to a specific area of the body through a round head probe. Sound waves move deep into the tissue (for example, in the muscles), creating gentle heat.
As the probe slides over the surface of the skin, sound waves penetrate the surface of the skin, causing soft tissue vibrations, creating heat. Instead, heat induces vasodilation: drawing blood into the target tissues.
Increased blood flow provides the necessary oxygen and nutrients and eliminates cellular waste. The heat helps relieve pain and inflammation, reduces muscle spasms, and accelerates healing. Depending on the treatment area, the range of motion may be increased.
Electrotherapy
Electrotherapy is an umbrella term that covers a series of therapies that use electricity, and which aims to reduce pain and improve muscle tension and function.
Electrotherapy usually involves the use of a battery-powered device that provides a current to the small electrodes (which attach to the patient's back). Electrodes send electrical impulses to your symptomatic back area. There are many types of electrotherapy devices available, but the most popular are transcutaneous electrical nerve stimulation units.
Although it rarely affects negatively, the side effects of electrotherapy may include skin irritation or rash. If you have torn skin or an infection, we recommend that you avoid using electrotherapy on those areas of the body.
Procedures that use diadynamic current
Diadynamic therapy is another term used for procedures with electrical stimulation. It is a single-phase impulsive current. The carrier frequency is a sine wave, which operates at 50Hz, which is then rectified (full-wave or half-wave). The resulting single-phase pulses last 10 milliseconds. The diadynamic current is conducted to the human body by cup or vacuum electrodes. There are several methods: trans-regional (at painful points on the affected nerve), paravertebral or segmental, and vasotropic.
The diadynamic current is contraindicated when presenting:
- acute inflammation
- malignant disease
- diseases that cause cachexia
- decompensated heart failure
- bleeding
- metal in the tissue (after injury, endo prosthetics, osteosynthesis, etc.)
Procedures that use interferential currents
Positive effects:
- Reduces or eliminates pain safely.
- Significant reduction of inflammation.
- Improves movement and coordination.
- Stimulates natural hormones that can help you heal faster.
- Considered by many experts as a very effective form of treatment for chronic pain.
![]()
Drug treatment for spondylosis
If regular medicines do not help, your doctor may prescribe: - Non-steroidal anti-inflammatory drugs. It is recommended to take ibuprofen or naproxen sodium to relieve pain and inflammation.
- Corticosteroids. Oral medications may help relieve pain. If your pain is severe, your doctor may suggest steroid injections.
- Muscle relaxant. Certain medications can help relieve muscle spasms.
- Anti-seizure drugs. Some types of epilepsy medications, such as gabapentin and pregabalin, can ease the pain of damaged nerves.
- Antidepressants. Certain antidepressant drugs are effective in reducing the pain caused by spondylosis.
Natural treatments to relieve spondylosis
Ginger: Ginger can be used as an anti-inflammatory. You can make ginger tea by adding a teaspoon of freshly grated ginger in hot water.
Surgical treatment for spondylosis
If conservative treatment fails or if neurological signs and symptoms - such as weakness in the arms or legs - worsen, you may need surgery to create more space for the roots of the spinal cord and nerves.The surgical treatment may involve:
- removal of a herniated disc or bone spines
- removal of part of some vertebrae
- merging a segment using the bone graft
Surgery for spondylosis involves two main components: removing the cause of the pain and then fusing the spine to control movement. When the surgeon removes the tissue that presses on a nerve, it is called a decompression operation. Fusion is a stabilizing surgery, and decompression and fusion are often performed at the same time.
![]()
Methods to prevent spondylosis
Long-term prevention or avoidance of any symptoms of spondylosis is the best option. This means a healthy lifestyle, exercise and endurance, aerobic exercise, work flexibility, and a strategic diet because they all help prevent such situations.
- Fitness: Work with your doctor to develop a safe workout plan for you. Try to include resistance training and aerobic exercise and flexibility in your routine.
- Lose weight: overweight or obesity puts pressure on the joints of the spine. This can speed up the normal process of wear and tear.
- Eat healthy and nutritious foods: base your diet on fruits, vegetables, and whole grains.
- Take breaks throughout the day: This is especially important if you work at the office all day. If possible, try to get up every 30 minutes to give your body a chance to stretch and relax.
- Good posture: sitting or standing correctly, promotes back health.
- Learn how to lift correctly: Proper lifting can help you avoid excessive back strain.
- Rest: Sleep goal of 8 hours per night.
- Stop smoking: Smoking can speed up the aging process and can affect the spine.
- Avoid excessive alcohol consumption: too much alcohol can lead to dehydration.
There is no sure way to say that you will completely avoid the development of spondylosis, but a healthy lifestyle is one of the best ways to prevent spondylosis.
Centrokinetic is the place where you will find clear answers and solutions for your motricity problems. The clinic is dedicated to osteoarticular diseases and is divided into the following specialized departments:
- Orthopedics , a department composed of an extremely experienced team of orthopedic doctors, led by Dr. Andrei Ioan Bogdan, primary care physician in orthopedics-traumatology, with surgical activity at Medlife Orthopedic Hospital, specialized in sports traumatology and ankle and foot surgery.
- Pediatric orthopedics , where children's sports conditions are treated (ligament and meniscus injuries), spinal deformities (scoliosis, kyphosis, hyperlordosis) and those of the feet (hallux valgus, hallux rigidus, equine larynx, flat valgus, hollow foot).
- Neurology , which has an ultra-performing department, where consultations, electroencephalograms (EEG) and electromyography (EMG) are performed.
- Medical recovery for adults and children , department specialized in the recovery of performance athletes, in spinal disorders, in the recovery of children with neurological and traumatic diseases. Our experience is extremely rich, treating over 5000 performance athletes.
- Medical imaging , the clinic being equipped with ultrasound and MRI, high-performance devices dedicated to musculoskeletal disorders, and complemented by an experienced team of radiologists: Dr. Sorin Ghiea and Dr. Cosmin Pantu, specialized in musculoskeletal imaging.
Find the latest news by following the Facebook and YouTube accounts of the Centrokinetic clinic.
SUCCESSFUL RECOVERY STORIES

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT