The Calf

The calf is the anatomical region located between the knee and ankle. It is formed by the tibia, located in the front, medially, and the fibula, located laterally.
These two bones are connected by the interosseous membrane and at the lower end form the two malleoli: the lower end of the tibia forms the medial malleolus and the lower end of the fibula forms the lateral malleolus. Among the largest muscles forming the calf are the anterior tibial in the front and the sural triceps in the back. Bone and muscle injuries are the most common at this level.
Contents
- Common Conditions
- tibia or fibula fracture
- muscle injuries
- Chronic Conditions
- stress fracture
- Surgical Interventions
- tibia or fibula fracture
Common Conditions
tibia or fibula fracture
- Based on the mode of fracture: traumatic or pathological (especially in the elderly due to osteoporosis or in the case of brittle bone disease)
- Based on the mode of occurrence: direct or indirect
- Based on the fracture pattern: transverse, oblique, spiral, or longitudinal
- Based on the bone fragments: compact or comminuted
- Based on skin involvement: closed or open (bone protrudes through the skin)
- Based on the extent of bone breakage: complete or incomplete (fissures)
- Based on fracture stability: stable or unstable
muscle injuries
.jpg)
A fracture is understood as an interruption of bone continuity. Fractures occur when the forces applied to a segment exceed its capacity to resist. There are several ways to describe a fracture:
Typical symptoms of a fracture include pain, joint stiffness, functional impotence, and hematoma. Diagnosis is usually confirmed by X-rays, and emergency treatment is provided as first aid.
After immobilization, it is very important to start a personalized recovery treatment. The initial recovery aims to reduce inflammation and pain, followed by increasing joint mobility and muscle strength. Gradual recovery of muscle strength and coordination is fundamental to achieving maximum functional recovery.
.jpg)
Muscle injuries are among the most common injuries in sports medicine. Most often they occur at the end of a tennis match, in the extra time of a football game, or at the end of an intense tournament when a feeling of fatigue in the muscles appears, but players continue to push themselves to finish the match. Muscle injuries can also occur following a serious clash while the player is in full action. Most often, these clashes force players to leave the field.
All these lead to the "famous" muscle injuries, which in most cases create confusion and distrust, but at the same time account for up to 30% of all sports injuries.
All activity interruptions bring up the famous questions:
- HOW LONG WILL IT TAKE TO RETURN TO WHAT I WAS DOING BEFORE?
- HOW LONG DOES RECOVERY TAKE?
First of all, it must be clear that what is presented in this material are just general treatment guidelines, which must be adapted to the particularities of each client and guided by a specialist doctor.
Muscle injuries can occur from direct contact (direct traumatic blows - contusions) or from a wrong movement (indirect trauma).
Contusions are easy to diagnose because it is known exactly when the trauma occurred, usually after direct contact with an opponent or an object. In these cases, depending on the functional incapacity caused by the contusion, they are defined as mild (range of motion is over 50% of normal), moderate (between 1/3 and half of the range), or severe (mobilization is difficult and no more than 1/3 of the range of motion). When we have severe contusions, the sooner you start physical therapy, the sooner you will resume the desired activities.
Classification of indirect trauma is much more complex.
If the pain is accompanied by an increase in muscle tone and occurs at the end of sports activity, it is most likely a muscle contracture with shortening. Conversely, if the pain is easy to localize, intensifies during sports activity, and makes activity difficult if not impossible, it is very likely to be a muscle strain. A muscle strain is not accompanied by an interruption of muscle continuity at the microscopic level. Even in this case, the faster you start recovery, the sooner it will take place.
Actual muscle tissue injuries (grade 1, 2, or 3) require longer recovery times. In these cases, we have a real anatomical injury that varies in severity depending on the amount of muscle tissue affected and its location. It is quite easy to identify a real muscle tear because the pain felt is acute and occurs after a specific technical gesture. You can even easily identify the location of the tear.
Functional impotence is directly proportional to the severity of the injury. Diagnosis is made by a clinical examination, but can be aided by an MRI scan done 24/48 hours post-trauma. Treatment must consider the grade and location of the injury and the patient's lifestyle. During the physical therapy program, the evolution can be monitored by muscle tissue ultrasounds and the location and size must be considered to avoid mistakes in recovery.
Chronic Conditions
stress fracture
.jpg)
Stress fractures are very common in performance athletes. They occur due to the repeated loading of the bone.
Diagnosis is made following a very precise clinical examination that takes into account changes in training style or loading during training. There are several predisposing factors that can increase the likelihood of a stress fracture, including exercising on hard surfaces, qualitative and quantitative variations in loading depending on sex and age.
The most affected by this type of fracture are long-distance runners, soldiers, and the elderly. Approximately 2-3 weeks after the initial fracture, the pain becomes unbearable and patients find no other solution but to completely, or almost completely, stop physical activity. Diagnosis must be made very carefully because there may be cases where the fracture is not visible on X-rays for 14-15 days. For this reason, a CT or MRI is recommended to confirm the diagnosis and evaluate its severity.
Treatment varies depending on the location and intensity of the fracture and can range from a short period of immobilization combined with the start of physical therapy, to long-term immobilization in a cast and in some cases even surgical fixation.
Surgical Interventions
tibia or fibula fracture
(4).jpg)
Emergency treatment for fractures of the tibia or fibula is provided by the specialist doctor as first aid. They will decide whether a fracture reduction or surgical fixation by an orthopedic surgeon is needed. After this, it is very important to start an early, personalized physical therapy program immediately after discharge.
BUCHAREST TEAM
CLUJ NAPOCA TEAM
BRASOV TEAM
MAKE AN APPOINTMENT
FOR AN EXAMINATION
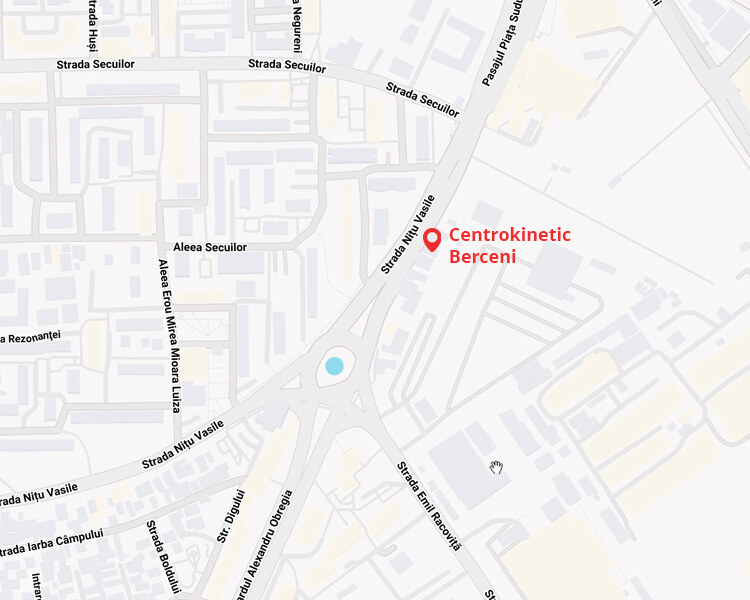
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT