
Discover the open MRI imaging center in our clinic. Centrokinetic has a state-of-the-art MRI machine, dedicated to musculoskeletal conditions, in the upper and lower limbs. The MRI machine is open so that people suffering from claustrophobia can do this investigation. The examination duration is, on average, 20 minutes.
Centrokinetic attaches great importance to the entire medical act: investigations necessary for correct diagnosis (ultrasound, MRI), surgery, and postoperative recovery.
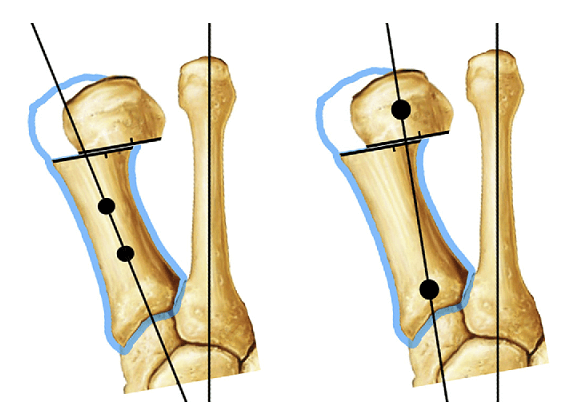
The bunion (hallux valgus) is one of the most common diseases of the forefoot, characteristic of women of all ages and much rarer in males. The bunions are characterized by the deviation of the thumb to the outside of the foot and the metatarsal I inwards, ie the patient must understand that no extra bone grows, but the disease eminently means a muscle imbalance, which leads to a deformity of bone position and ratios.
.jpg)
.jpg) | .jpg) |
The condition occurs bilaterally, often with an unknown cause, and less often unilaterally when following pes valgus. However, from our experience we can tell that there are clear causes that determine the appearance of bunions: hereditary factors, inadequate footwear associated or not with excess weight, prolonged orthostatism, rheumatoid diseases such as rheumatoid arthritis, congenital or acquired diseases such as flat feet.
Treatment depends primarily on the symptoms. Patients suffering from bunions must understand that the treatment is eminently surgical, but this treatment has no aesthetic indication.
 |
There is no proven benefit, both in the early stages of the disease and in the advanced stages, offered by wearing various dispensers or assistive devices sold in the market. These devices have a well-established postoperative role in allowing the tissues to heal.
However, we can think of a prophylactic treatment through sports, medical gymnastics, proper footwear, and hygiene.
The treatment of choice is the surgical one, and the indication appears when the patient has significant pain and real difficulties when standing for long periods.
Surgical technique
There are several surgical techniques, and the optimal choice depends on the type and degree of deformation, but also on the associated or secondary lesions after the development of the bunions.
- Distal osteotomy (Chevron technique): involves "V" sectioning of the MTS (metatarsal) I neck, bone realignment by more lateral repositioning of the MTS head and fixing it in the new position with 1 Herbert screw. This technique effectively reduces the angle between the first and second metatarsal bone and retracts the proximal phalanx and sesamoid bones on the head of the metatarsal I. This type of procedure requires an incision of about 2 cm at the base of the thumb.
- Osteotomy at the level of the MTS I diaphysis (Scarf technique): involves the inverted "Z" sectioning of the diaphysis of the first metatarsal, the lateralization of the dorsal bone, and the fixation with 2 Herbert screws. This type of procedure usually requires a single incision of about 4-5cm. Again, this procedure reduces the angle between the first and second metatarsal bone, and ensures realignment of the thumb in the case of an advanced bunion, then associating the release of tense structures on the side of the joint. This procedure includes the joint capsule and the adductor hallucis muscle tendon. This muscle tends to pull the thumb inward. By releasing the tendon, the finger no longer moves. The toe is realigned and the joint capsule on the medial side of the thumb is tense to keep the foot straight.
- Lapidus arthrodesis: in case of very advanced deformities, we recommend a surgical technique that blocks the cuneiform-metatarsal joint (at the base of the first ray), with the help of which we realign MTS I.
- Metatarsophalangeal arthrodesis: in case of very advanced deformities, associated with osteoarthritis of the joint at the base of the thumb (metatarsophalangeal), we recommend a surgical technique that blocks this joint, with which we realign MTS I and the big toe.
Postoperatively
After the operation, the patient remains hospitalized for 1 day. He will receive pain medication and antibiotics during his hospitalization. The operated limb is not immobilized in a plaster splint and the patient is advised to make ankle and foot exercises from the first postoperative day under the supervision of physical therapists. Walking is allowed with the help of a stabilizing orthesis, being necessary to use crutches, even in the conditions in which the chosen intervention was minimally invasive.
.jpg)
Patients will wear a compressive bandage on the foot for 5 days. Patients can return to family and professional activities quickly, up to 3-4 weeks, if they have office work, and 12 weeks, if they have fieldwork.
At home
Although recovery after this operation is much faster than a classic intervention, it will still take a few weeks for you to fully recover the operated joint. You should expect pain and discomfort for at least a week postoperatively. You can use a special ice pack, which will reduce the pain and inflammation. You must be careful not to lean on the operated area in the first weeks because the pain and discomfort can worsen. You can take a bath, but without wetting the bandage and incisions. The threads are suppressed at 14 days postoperatively. At 6 weeks postoperatively, an MRI is necessary to see how the tendon suture heals. Driving is allowed after 8 weeks, and hard physical work after 10-12 weeks.
Physical therapy plays a very important role in the rehabilitation program, and the exercises must be followed by a physical therapist until the end of the recovery period.
It is very important to follow the recovery program strictly and seriously for the surgery to be a success. Our medical team works on average with the patient after this intervention, 12-16 weeks until complete recovery of the operated area.
Following any surgery, medical recovery plays an essential role in the social, professional, and family reintegration of the patient. Because we pursue the optimal outcome for each patient entering the clinic, recovery medicine from Centrokinetic is based on a team of experienced physicians and physical therapists and standardized medical protocols.
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT





































































































































