.jpg)
For all traumatic or chronic diseases of the musculoskeletal system, the Centrokinetic private clinic in Bucharest is prepared with an integrated Orthopedic Department, which offers all the necessary services to the patient, from diagnosis to complete recovery.
The Department of Orthopedic Surgery of Centrokinetic is dedicated to providing excellent patient care and exceptional education for young physicians in the fields of orthopedic surgery and musculoskeletal medicine.
Centrokinetic attaches great importance to the entire medical act: investigations necessary for correct diagnosis (ultrasound, MRI), surgery, and postoperative recovery.
Discover the open MRI imaging center in our clinic. Centrokinetic has a state-of-the-art MRI machine, dedicated to musculoskeletal conditions, in the upper and lower limbs. The MRI machine is open so that people suffering from claustrophobia can do this investigation. The examination duration is, on average, 20 minutes.
Located outside the knee joint, the posterolateral corner (PLC) works to stabilize the knee against direct or lateral direct forces. Injuries in this area are often caused by sports, such as football, rugby, handball, skiing, and basketball. Although injuries in this area of the knee represent a lower percentage of cases compared to injuries of the anterior cruciate ligament (ACL) or medial collateral ligament (MLC), this injury can have a devastating impact on athletic performance.
The posterolateral corner of the knee is one of the most complex areas, both in terms of diagnosis and in terms of surgical treatment options.
Symptoms of a PLC injury include:
- Frontal instability
- Difficulty twisting, rotating, and pivoting
- Local swelling
- Pain in the side of the knee
- Lack of dorsiflexion of the foot, in case of damage to the common peroneal nerve.
Patients gradually notice the onset and worsening of instability in the following weeks or months after the trauma, if they do not reach the orthopedist immediately after the injury. This is problematic because the ideal result is obtained if the surgery is performed in the first 2-3 weeks after the initial injury.
.jpg)
The main anatomical structures of the posterolateral corner of the knee are:
- lateral ligament (fibular)
- collateral ligament (LCL)
- popliteal muscle tendon
- popliteofibular ligament.
In addition, the lateral capsule, with the thickening called the anterolateral ligament and the insertion of the femoral biceps muscle on the fibula head, serve as very important stabilizers of the knee. At the same time, with these ligaments, it is very important to evaluate the function of the common peroneal nerve, because the nerve has an anatomical trajectory along the neck of the fibula, very close to these structures. Approximately 15-20% of patients may have a nerve injury with numbness or impaired ankle mobility.
Diagnosis of posterior knee injuries
There are several tests needed to diagnose a posterolateral elbow injury of the knee. These include:
- Varus stress test - is performed in full extension and at 30 knee flexion
- Dial test - at 30 and 90 at knee flexion
- Posterolateral drawer test
- External rotation test in the recurvatum
- Reverse Pivot Shift Test
.jpg) | .jpg) | 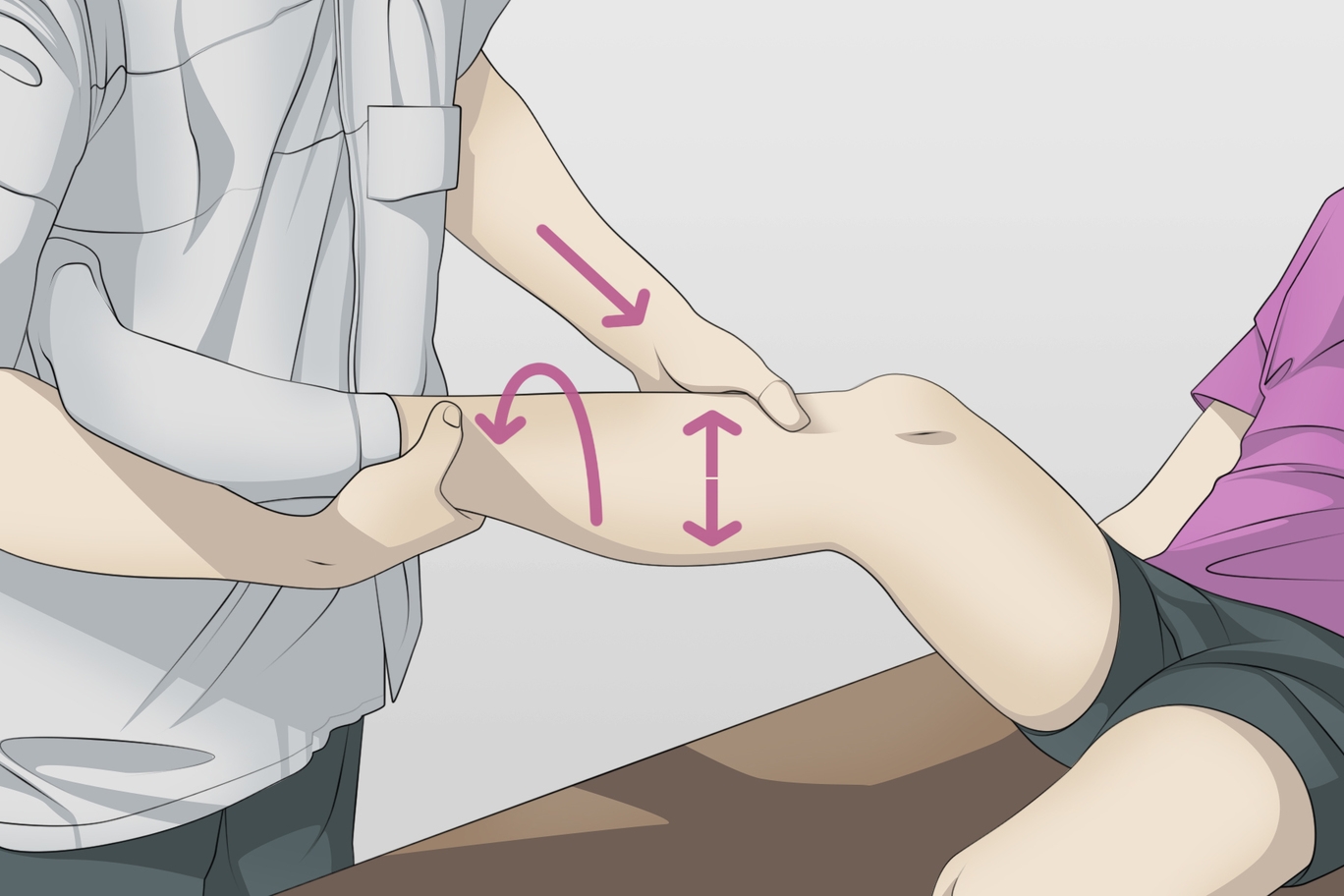 |
All of these tests should be made to determine the type of instability present in the knee, and during the clinical examination, the tests should be applied to both legs to have a comparative term. In acute cases, these tests can be extremely painful, and patients may become tense, situations in which imaging (MRI) becomes extremely important. Approximately 72% of patients who have a PLC lesion will also have a concomitant lesion of the anterior cruciate ligament. Thus, we must not overlook the possibility of a posterolateral corner injury by focusing only on the affected cruciate ligament, because failure to diagnose this lesion will cause a failure of ligamentoplasty.
.jpg) | .jpg) | .jpg) | .jpg) |
Posteroexternal knee injuries are classified as follows:
- Grade I: small partial lesion with minimal instability
- Grade II: partial injury, with instability in flexion of 30 degrees
- Grade III: complete lesion with instability both in flexion and extension
In general, noi recomandam ca toate leziunile de gradul III sa fie abordate chirurgical, datorita probabilitatii scazute de vindecare. Acest lucru se datoreaza in primul rand anatomiei unice a coltului posterolateral - sunt prezente doua suprafete osoase convexe opuse care conduc la o instabilitate osoasa inerenta.
We recommend that all grade III lesions be treated surgically due to the low probability of cure. This is primarily due to the unique anatomy of the posterolateral corner - there are two opposite convex bone surfaces that lead to inherent bone instability.
In general, due to the high risk of scarring and withdrawal of broken structures, we recommend that surgery be performed within two to three weeks after trauma, to allow rapid resumption of movement through physical therapy.
The surgical technique performed by our team:
An incision of about 7 cm is made in the lateral area of the knee, the iliotibial tract, the femoral biceps muscle, and the common peroneal nerve are highlighted, which are isolated. The iliotibial tract is incised and the lateral femoral epicondyle is highlighted. 2 bone tunnels are made with a distance between them of 18mm and a diameter of 6mm.
Subsequently, the head of the fibula is highlighted and a 6mm oblique anteroposterior canal is made. Another posteroanterior canal is made through the tibia, using a special guide, with a diameter of 9mm and a length equal to the diameter of the tibia.
The semimembranosus muscles of both legs are harvested, fixed in the femoral canals with 2 7 / 25mm screws, then the tendon fixed in the posterior femoral canal is brought on the iliotibial tract and fixed in the fibula head with 1 6mm screw in 20 degrees of flexion, and at the end, both tendons left free are fixed in the tibia with a 10mm screw in 60 degrees of flexion.
.jpg)
The surgery is complex, laborious, and requires a lot of experience from the medical team, things that the Centrokinetic team offers having a vast experience in knee surgery.
The operation is performed under spinal or general anesthesia, with 1 or 2 nights of hospitalization, and recovery begins the next day.
Postoperative recovery for these lesions includes flexion movements 0-90 degrees in the first two weeks, then the amplitude of flexion increases progressively to 8 weeks. Patients use a mobile knee orthosis for 8 weeks and do not load the operated limb for 6 weeks. Full recovery takes an average of 9 months.

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT




































































































































