Discover the open MRI imaging center in our clinic. Centrokinetic has a state-of-the-art MRI machine, dedicated to musculoskeletal conditions, in the upper and lower limbs. The MRI machine is open so that people suffering from claustrophobia can do this investigation. The examination duration is, on average, 20 minutes.
Centrokinetic attaches great importance to the entire medical act: investigations necessary for correct diagnosis (ultrasound, MRI), surgery, and postoperative recovery.
The Lisfranc joint is the point where the metatarsal bones (long bones that lead to the toes) and the tarsal bones (arched bones) articulate. The Lisfranc ligament is a hard band of tissue that joins two of these bones, and has a very important role in maintaining proper alignment and resistance of the anatomical area to the forces that appear when walking, but also in intense physical activity.
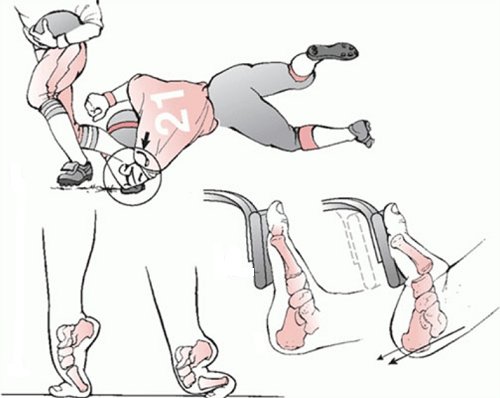
Lisfranc joint injuries occur most frequently as a result of road accidents, but also in military personnel, runners, riders, football players, and contact sports participants. Lisfranc injuries occur as a result of direct forces (crushing of the foot by a blunt object) or indirect forces (twisting of the foot) acting on the forefoot.
Types of Lisfranc injuries:
Three types of Lisfranc lesions sometimes occur together:
- Sprains: The Lisfranc ligament and the other ligaments on the lower part of the midfoot are stronger than those on the upper part, so an abnormal movement can cause mediotarsal dorsal instability.
- Fractures: may occur in the first part or may involve other parts of the midfoot. At other times, they may appear as simple bone snatches.
.jpg)
- Dislocations: the bones of the Lisfranc joint can be displaced from their normal positions, and the ligament can give way completely, appearing the Lisfranc dislocation.
.jpg)
Up to 20% of Lisfranc lesions go unnoticed or are diagnosed late, especially low-energy lesions or ligament lesions. Severe sequelae such as post-traumatic osteoarthritis and leg deformities can create a severe disability.
Conservative treatment is indicated only in stable and non-moving injuries, along with immobilization and initial avoidance of weight loading.
Through surgical treatment, we seek to achieve two objectives: optimal anatomical reduction, a factor that directly influences the results and stability of the first, second, and third cuneiform metatarsal joints.
There are three main controversies regarding the surgical treatment of Lisfranc lesions:
- osteosynthesis versus primary arthrodesis
- transarticular screws to the backplates
- the most appropriate surgical approach
The surgical treatment we prefer is open reduction and internal fixation (ORIF) with transarticular screws or dorsal plates in cases of communicative fractures of the metatarsals or cuneiform bones.
Surgical technique
The patient is placed in a supine position and we make an incision of about 4 cm centered on the intermetatarsal space I. If there is an impairment of the third metatarsal or the instability of the fourth or fifth metatarsal, we use a double approach, making a longitudinal incision in the first inter-metatarsal space and another longitudinal incision according to the fourth metatarsal.
.png)
We make a reduction of the bones from the medial to the lateral part. We start by reducing the first cuneiform metatarsal joint with K brooches and fixing the bones with two 3.5 mm titanium screws, from the first metatarsal to the first cuneiform. Then, we use a second screw from the first wedge to the first metatarsal.
The next step is to reduce the space between the first and second metatarsals. For this purpose, we use a reduction clamp between the median area of the first cuneiform bone and the lateral area of the second metatarsal and perform bone fixation with a non-cannulated screw of 4 or 4.5 mm from the first cuneiform to the base of the second metatarsal. The next screw goes from the second metatarsal to the second cuneiform once the joint has been reduced.
.png)
Through the incision on the fourth metatarsal, the third tarsus-metatarsal joint is evaluated and reduced, if necessary. Bone fixation is performed with two 3.5 mm titanium screws or a 3.5 mm screw and a K buckle. Practically, each joint must be stabilized with two screws or a screw and a brooch.
If there is an impairment of the fourth and fifth metatarsals, they will be stabilized with K brooches, which are to be removed six weeks postoperatively.
.png) | .png) |
If there is a fracture of the metatarsal bases or cuneiform bones, we use dorsal plates to stabilize the corresponding joint. However, we always use the one known as the "Lisfranc screw" between the first cuneiform bone and the base of the second metatarsal.
If the initial lesions have been neglected and the lesions are chronic (over 30 days), the surgical technique we opt for is cuneiform-metatarsal or cuboid-metatarsal arthrodesis. We remove these unstable joints and fix them with titanium backplates and screws.
Postoperatively
After the operation, the patient remains hospitalized for 1 day. He will receive pain medication and antibiotics during his hospitalization. The operated limb is immobilized in a plaster splint, and the patient is advised not to make ankle movements, 60 days after the intervention. When walking, is necessary to use crutches, even if the chosen intervention was minimally invasive.
Patients will wear a compressive bandage on the foot for 5 days. Patients can return to family and professional activities quickly, up to 3-4 weeks, if they have office work, and 12 weeks, if they have fieldwork.
.png)
At home
Although recovery after this operation is much faster than a classic intervention, it will still take a few weeks for you to fully recover the operated joint. You should expect pain and discomfort for at least a week postoperatively. You can use a special ice pack, which will reduce the pain and inflammation. You must be careful not to lean on the operated area in the first weeks because the pain and discomfort can worsen. You can take a bath, but without wetting the bandage and incisions. The threads are suppressed at 14 days postoperatively. At 6 weeks postoperatively, an MRI is necessary to see how the tendon suture heals. Driving is allowed after 8 weeks, and hard physical work after 10-12 weeks.
Physical therapy plays a very important role in the rehabilitation program, and the exercises must be followed by a physical therapist until the end of the recovery period.
It is very important to follow the recovery program strictly and seriously for the surgery to be a success. Our medical team works on average with the patient after this intervention, 12-16 weeks until complete recovery of the operated area.
Following any surgery, medical recovery plays an essential role in the social, professional, and family reintegration of the patient. Because we pursue the optimal outcome for each patient entering the clinic, recovery medicine from Centrokinetic is based on a team of experienced physicians and physical therapists and standardized medical protocols.
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT