.jpg)
.jpg) | .jpg) |
Drug treatment of articular cartilage lesions
Glucosamine and Chondroitin Sulfate
Glucosamine (2-amino-2-deoxy-alpha-D-glucose) and Chondroitin Sulfate (a long, unbranched polysaccharide composed of alternative residues of glucuronic acid and N-acetylglucosamine) have chondroprotective properties.
Both substances are components of proteoglycan complexes in chondrocytes.
Hyaluronic acid
Hyaluronic acid is a polysaccharide with viscoelastic properties that improves lubrication and joint mechanics. Although the mechanisms of action of hyaluronic acid are not fully understood, it modulates cellular metabolism and has a chondroprotective effect. We recommend infiltrations with Optivisc Single (3%).
Glucocorticoids
Injectable glucocorticoids have long been used to treat osteoarthritis. Although they are effective in reducing symptoms, their effect is limited to a few weeks. Although glucocorticoids appeared to have a protective effect, most experimental data suggest that they have a negative effect on cartilage biology by inhibiting chondrocyte proliferation, decreasing matrix synthesis, and proteoglycan synthesis.
Non-steroidal anti-inflammatory drugs
These are the most prescribed painkillers in the treatment of joint cartilage injuries. The effectiveness of nonsteroidal anti-inflammatory drugs is mainly due to the inhibitory effect on COX-2. Cyclooxygenase-2 stimulates tissue catabolism while decreasing the synthesis of type II collagen and proteoglycans. However, there is no evidence that it would delay the progression to osteoarthritis. Among the NSAIDs we mention: Arcoxia, Voltaren, Diclofenac, Ketoprofen.
.jpg)
Platelet-enriched plasma infiltrations: is one of the most effective non-surgical methods of treatment, with a practice in Austria and the USA for over 30 years. The treatment is relatively simple, with minimal risks. The procedure involves collecting peripheral (venous) blood in a special container, in a quantity varying between 60-120 ml, depending on the purpose of the therapy. Subsequently, the blood obtained is centrifuged, thus obtaining the separation of blood cells and platelets containing regenerating factors. They are injected in the same session in the joint.
Surgical treatment of articular cartilage lesions
Several factors must be considered to decide to treat joint cartilage injury: surface area, depth, location, history, associated injuries, knee stability, meniscal injuries, mechanical limbs, patient age, and last but not least functional characteristics of the patient. MRI examination, Outerbridge Classification, ICRS Assessment System are very useful for choosing the therapeutic method. Regarding the repair of cartilage lesions along with the entire thickness, several treatments have been suggested, but none have been identified as the "gold standard" to allow the reproduction of normal hyaline joint tissue. One of the first treatments is simple abrasive chondroplasty when the cartilaginous defect is "shaved" and subjected to extensive debridement.
Washing and Debridement of articular cartilage
These arthroscopic techniques have proven useful for patients with reduced mechanical stress on the joint and unique and relatively small lesions on the surface and who do not wish to undergo long-term recovery treatment. The results obtained are relatively low by the isolated use of this method. These are techniques performed in an arthroscopy, along with other surgical techniques.
Blast stimulation techniques
Bone marrow stimulation has proven to be a useful technique, with good results. Bone marrow stimulation includes a group of techniques that cause bleeding of the subchondral bone at the level of the lesion with the addition of blasts, which will form fibrocartilage. The advantage of these techniques is related to the simplicity of performance, common instrumentation available to any surgeon, and the short time required to perform. The main disadvantage is related to the repair of the cartilaginous defect by fibrocartilage, which limits in time the result obtained due to the inferior properties of the fibrocartilage compared to the hyaline cartilage.
- Pridie drilling
After the publication of the Pridie technique in 1959, it became widely used, being simple to perform and does not require special tools. The technique aims to make holes in the bone bed of the lesion to cause bleeding.
- Steadman microfractures
.jpg) | .jpg) |
Autologous Osteochondral Transplant
Another treatment technique includes transplanting an osteochondral cylinder, taken from an area that is not subject to loading, into the defect through a one-time operation (OATS: Osteochondral Autologous Transplantation). Autologous Osteochondral Transplantation is a procedure in which one or more osteochondral cylinders are taken from a donor area and implanted in the area of the cartilaginous defect. Technically, several osteochondral cylinders are harvested from an unimportant area of the knee - a variable number and of variable dimensions, to cover the surface of the defect as well as possible - with a special instrument.
.png)
The advantages of the technique consist in the possibility of performing in a single operative time, even if there are lesions of the subchondral bone (osteochondritis, degenerative lesions), they are low cost, slower recovery time compared to the autologous chondrocyte implant. The disadvantages of the method consist mainly in adverse effects related to the donor area and the limitation of the surface that can be covered due to the limitation of the area where cylinders can be harvested.
The main current indication of this technique is for chondral defects in the femoral condyles with an area of 2-4 cm2, in active patients, but also active elderly patients depending on the condition of the cartilage in the rest of the joint.
Autologous Chondrocyte Implantation (ACI)
The implantation of autologous chondrocytes was first described in 1994 by Brittberg et al. It is a method by which the regeneration with hyaline cartilage (hyaline-like) is achieved with the help of chondrocytes cultured in vitro, a method increasingly used. The technique involves a first intervention by which chondrocytes (200-300 mg) are harvested for cultures and after their development in vitro; a new surgery that fills the cartilaginous defect with these cells, their contention in the defect being achieved with the help of periosteal or collagen membranes.
Long-term results do not yet exist, but medium-term studies show 80-85% good results. The advantage of the method is the low invasiveness of the technique, without adverse effects at the site of chondrocyte harvesting, but it requires a good quality subchondral bone, which reduces its indications. The main disadvantage of the method is the high price: 8,000-10,000 EUR for a patient. The technique also involves two surgeries, a longer learning curve for suturing the periosteal membrane or collagen under which chondrocytes are injected. This technique has been used more than the second and third-generation techniques, where we prefer to use more scaffolds in the membrane model, to maintain the initial tissue growth and provide a layer for cell culture.
AMIC (Autologous Matrix Induced Chondrogenesis) technique
In 2004, Behrens et al introduced a technique called AMIC (Autologous Matrix Induced Chondrogenesis), in a single operative time combining microfractures with collagen membrane lining, to stop the migration of mesenchymal cells to the subchondral bone exposed by microfractures, protecting blood clots and keeping stem cells at a fixed point, since they help differentiate the processes by which tissue is restored.
.jpg)
Although the AMIC technique is well established when treating cartilage defects, only a few studies have been published in the literature. When researching the AMIC procedure in 27 patients, Gille et al reported significant improvements in all clinical outcomes, with 87% of patients satisfied with post-surgical outcomes. However, magnetic resonance imaging showed that the "filling" of the defects was moderate to complete, with a normal signal, which is typically hyperintense.
In 2012, Kusano et al reported in a study that included a follow-up period, significant improvements in clinical outcomes, especially osteochondral defects. However, magnetic resonance imaging did not show complete or homogeneous restorations of cartilage defects. In 2013, Gille et al published the results of the AMIC technique and concluded that this technique is safe and effective. But research is needed over a longer period to determine whether the area undergoing treatment will retain its structural and functional integrity over time.
Thus, small modifications of the original technique were made. In 2011, Dhollander et al described the details of the "AMIC plus" technique, introducing platelet-rich plasma into the treatment of patellar cartilage defects, and concluded that it may be indicated for the treatment of patellar defects, helping to improve the clinical outcomes of all patients. , except for magnetic resonance imaging, where the number of patients with complete restorations was more limited. In addition to hematopoietic stem cells, bone marrow also contains a significant number of mesenchymal stem cells and is a rich source of growth factors, including PDGF (Platelet-derived growth factor), TGF-р (Transforming growth factor- and VEGF (Vascular endothelial).
The use of bone marrow concentrate in combination with microfractures has shown improvements in the treatment of lesions in horses, as well as in goats. In the first case, research of the group of horses treated with microfractures and bone marrow concentrate, compared to the group treated only with microfractures, demonstrated a significantly better tissue regeneration for the first group. In Saw's work with goats, the group of animals that were treated with post-surgical injections following subchondral perforation with hyaluronic acid and bone marrow concentrate showed almost complete healing of osteochondral defects, with the regeneration of hyaline articular cartilage.
Postoperatively
MAKE AN APPOINTMENT
FOR AN EXAMINATION
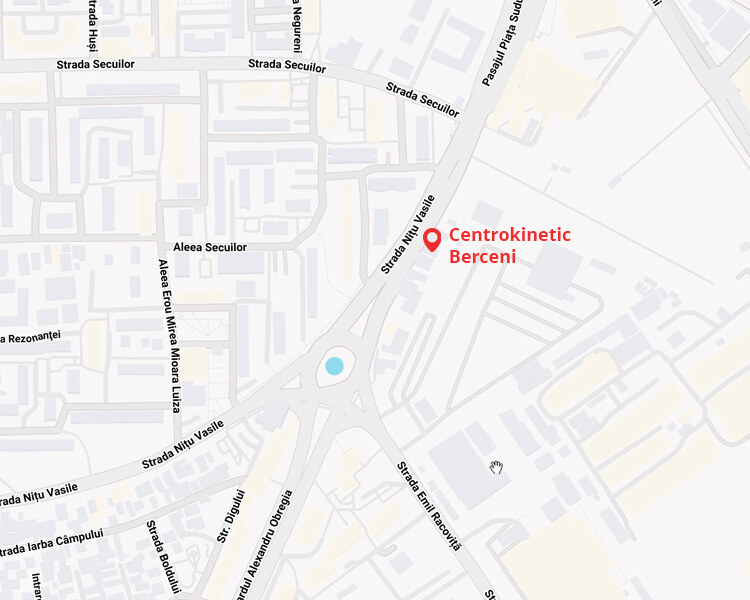
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT