.jpg)
For all traumatic or chronic diseases of the musculoskeletal system, the Centrokinetic private clinic in Bucharest is prepared with an integrated Orthopedic Department, which offers all the necessary services to the patient, from diagnosis to complete recovery.
The Department of Orthopedic Surgery of Centrokinetic is dedicated to providing excellent patient care and exceptional education for young physicians in the fields of orthopedic surgery and musculoskeletal medicine.
Centrokinetic attaches great importance to the entire medical act: investigations necessary for correct diagnosis (ultrasound, MRI), surgery, and postoperative recovery.
Discover the open MRI imaging center in our clinic. Centrokinetic has a state-of-the-art MRI machine, dedicated to musculoskeletal conditions, in the upper and lower limbs. The MRI machine is open so that people suffering from claustrophobia can do this investigation. The examination duration is, on average, 20 minutes.
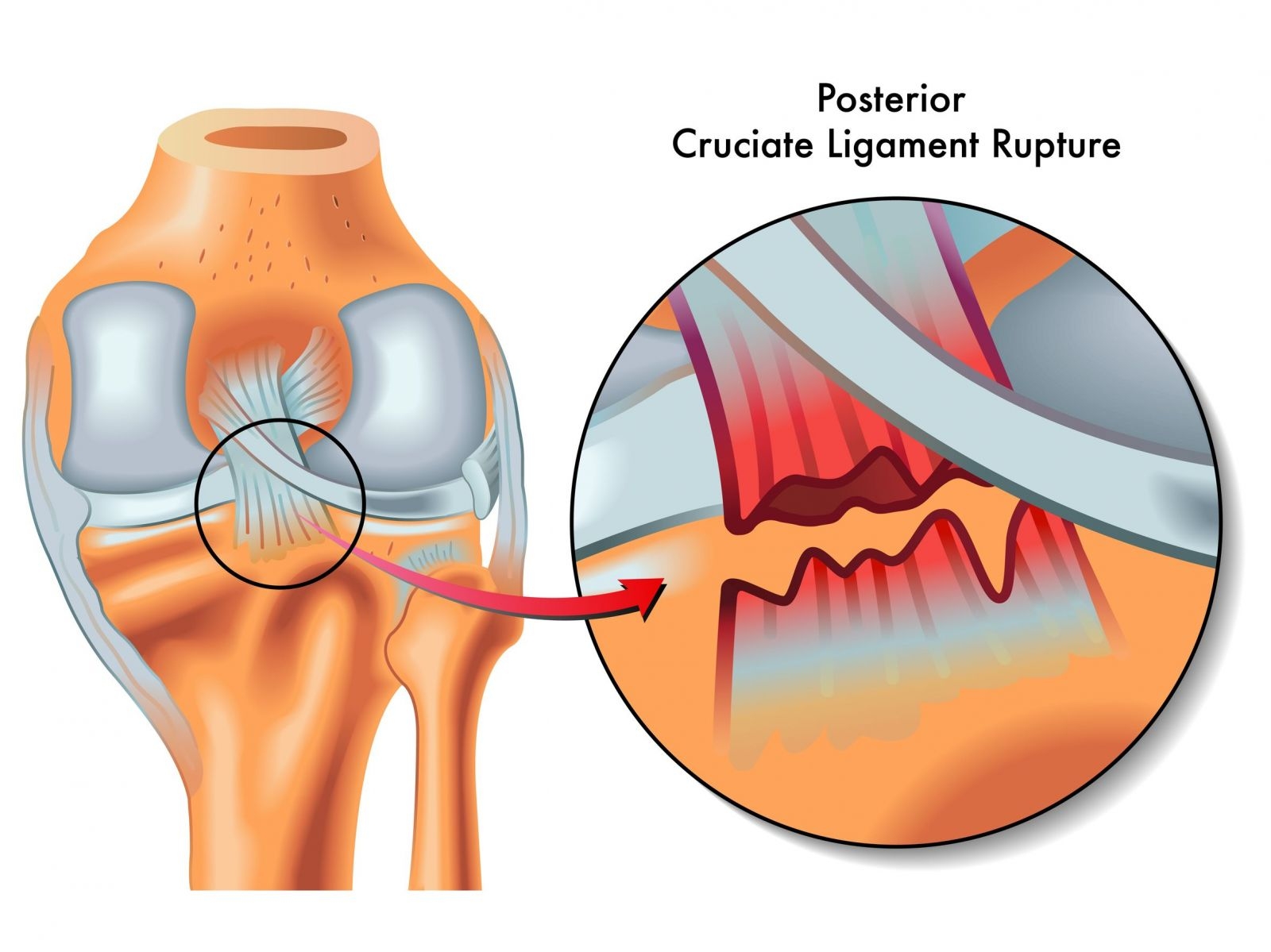
The posterior cruciate ligament (PCL) is described by many authors as the main stabilizer of the knee.
PCL lesions are much rarer than those of the anterior cruciate ligament, and can often go unnoticed. PCL is thicker and stronger than ACL and can withstand a tensile force of 2000 Newtons. Injuries most commonly occur when a force is applied to the anterior portion of the proximal tibia, with the knee flexed. Hyperextension and rotation as well as varus / valgus deformities may be responsible for PCL ruptures. PCL rupture can occur in isolation, the ligament being the only damaged element, or together with other ligament injuries. A rupture of the PCL can cause varying degrees of disability, ranging from no symptoms to severe patient disabilities.
The main function of PCL is to prevent posterior translation of the tibia into the femur. PCL also plays an important role as the central axis of the lower limb, controlling and imprinting the rotational stability of the knee. This lesion has not received sufficient attention and recognition in the past, compared to ACL lesions, but the increasing incidence of this pathology has increased attention to these lesions, today being increasingly studied. However, there is controversy in the literature regarding the treatment of isolated PCL lesions, and there are recommendations that support both surgical and conservative treatment.
.jpg)
There are three different opinions regarding the surgical approach to LIP ligamentoplasty. The debates are made regarding the choice of the type of graft, the positioning of the tibial and femoral tunnels, the number of bundles of the graft (thickness of the graft), and the tension applied to the graft.
Grafts can be represented by:
- allograft (usually Achilles tendon grafts)
- autografts (BTB - bone-tendon-bone, hamstring, or quadriceps muscle graft).
The most used autograft is represented by BTB because the bone "plugs" allows sufficient fixation of the tissue. The disadvantages of the graft are the morbidity of the harvest site (pain, fibrosis, flexion limitation, patellar tendon retraction) and the fact that, because the graft has a rectangular shape, the tunnels cannot be filled with collagen. The use of the hamstring tendon decreases the morbidity factor, but it is an inferior reconstruction method. The quadriceps muscle tendon also has increased morbidity at the harvest site, but the biomechanical properties of the knee following surgery are very satisfactory.
Allografts ensure a shorter surgical time and the absence of iatrogenic trauma at the harvest site. The Achilles tendon graft produces an increased amount of collagen, thus guaranteeing a complete filling of the tunnels.
When we use a graft with two bundles, we can reconstruct the two bundles of PCL, anterolateral and posteromedial. In the case of a single-beam graft, only the reconstruction of the stronger anterolateral beam will be performed. The two-beam approach will restore the normal kinetics of the knee, with a full range of motion, instead, it is a more invasive technique involving 2 femoral channels instead of one.
Surgical technique
In our team of orthopedists, for the reconstruction of the LIP rupture, we use the all-inside reconstruction technique with the help of a graft made from the tendons of the gracillis and semitendinosus muscles or the quadriceps tendon. We obtained great results using artificial LARS.
Transplant preparation
The graft is prepared using a special mass, which keeps it in tension at both the femoral and tibial ends, with the help of special sutures called TightRope. The graft is folded in 4 and sutured with a FiberWire suture. Then, the graft is marked at 25 mm, both in the femoral and in the tibial part, for the intraoperative evaluation of the graft positioning in the femoral and tibial tunnels. The length of the graft should normally be 80-100 mm, but a much more important parameter is the thickness of the graft, given that LIP is a thicker and stronger ligament than LIA.
Tibial canal preparation
After a standard diagnostic arthroscopy, an accessory posteromedial portal is made to expose the tibial imprint of the PCL. The PCL guide is inserted through the anteromedial portal and is positioned at the base of the ligament tibial abutment. If necessary, the correct location of the guide can be confirmed with fluoroscopy. Then, a FlipCutter is inserted from the anterior to the posterior, through the tibia, until the drill penetrates the posterior cortex. The PCL guide is used to prevent the FlipCutter from plunging into the posterior neurovascular structures. The next step is to make the tibial tunnel using the same FlipCutter, with a depth of at least 35-40 mm, which is cleaned with a shaver. Passage sutures are placed in the canal and are pulled through the joint, and then through the anteromedial and anterolateral portals.
.png) | 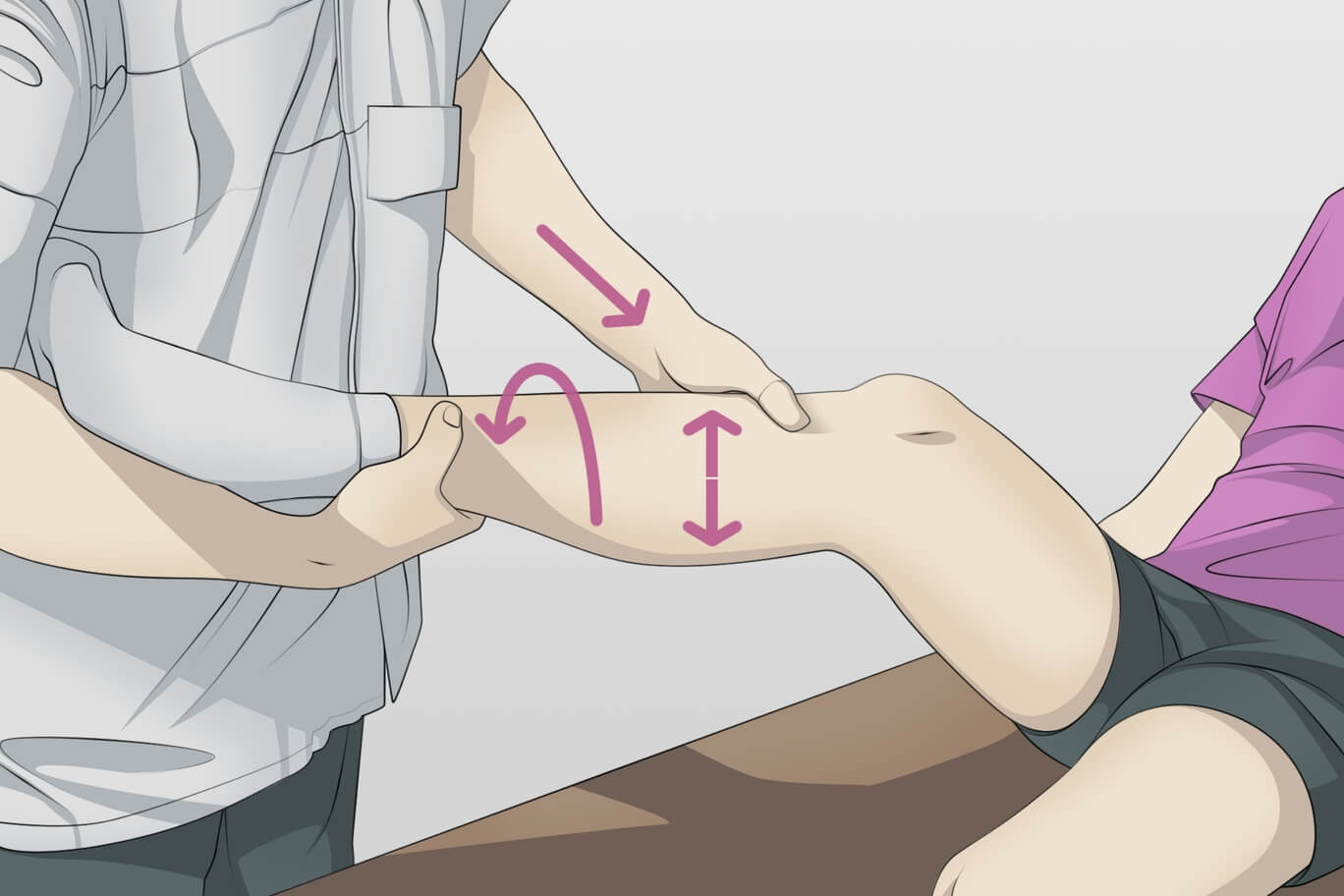 | .png) |
The native femoral imprint of the PCL is exposed and some fibers are preserved to help place the femoral tunnel. A guide is inserted through a distal inferolateral accessory portal and inserted in the center of the anatomical imprint of the PCL. An 11 or 12 mm cannulated reamer is passed over the guide and positioned at the most distal and anterior edges of the impression. This avoids the risk of cartilage damage because the reamer acts practically as a guide. Then, the femoral tunnel is reamed to a depth of at least 25 mm. Similar to the femoral part, a passage suture is placed for the graft passage.
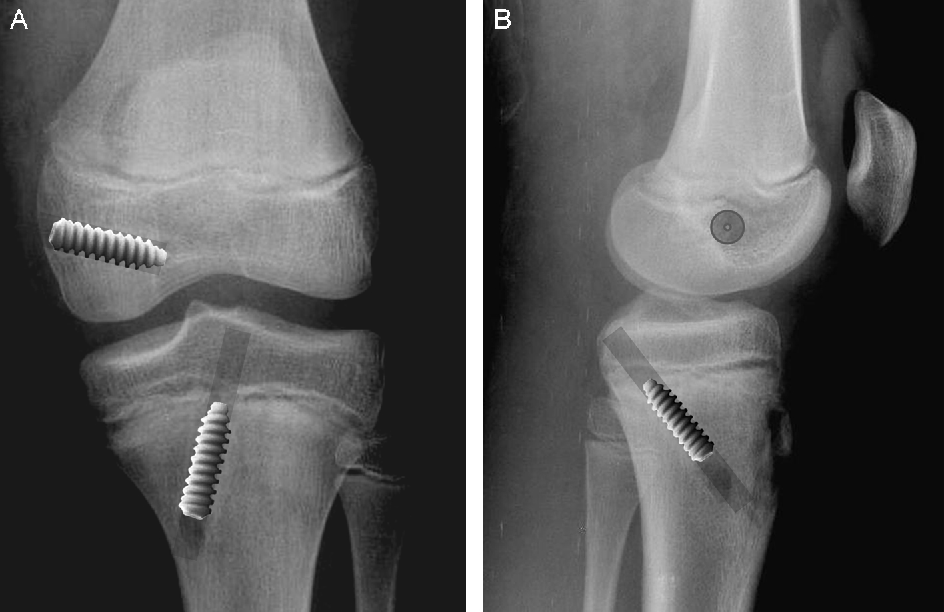
.jpg)
Fixing the graft
The passing sutures of the tibial and femoral parts are pulled through an inferolateral accessory portal. These sutures should be wrapped around TightRope sutures, which were previously sewn during graft preparation. We prefer to pass the graft through the tibial tunnel first, which allows the entire graft to be in the knee joint before it is finished. reconstruction. Then, we pull the graft into the femoral tunnel, while maintaining tension on the TightRope sutures. TightRope sutures should be tightened so that the graft sits at a depth of at least 20 mm in the femoral tunnel. Then, the arthroscope is placed in the posteromedial portal and the tibial portion of the graft is visualized to ensure that the depth of the graft in the tibial tunnel is at least 20 mm. If there is an excess of length, the TightRope suture can be tightened on the femoral side, pulling the graft further into the femoral tunnel. With the knee flexed at 80-90 degrees, secure and tension an Attachable Button System (ABS) on the tibial TightRope. Tensioning the TightRope on the femoral side is the last step in fixing the graft in both the femoral and tibial tunnels.
The main purposes of all-inside PCL reconstruction remain the same:
- accurately reconstructing the PCL within the native fingerprint,
- recreating normal anatomy
- restoration of ligament stability and complete restoration of range of motion and knee function.

In terms of these factors, the all-inside PCL reconstruction technique has many advantages. By using smaller incisions, the all-inside technique is much less invasive and can shorten the operating time by making the femoral tunnel with the help of arthroscopic assistance. In addition, the all-inside technique is particularly useful in multi-ligament reconstructions, at the same time, allowing the avoidance of neuro-vascular structures using the retrograde tunneling technique, which leads to a decrease in the amount of bone mass removed, unlike the tunnel. traditional. This facilitates increased retention of the host bone and also reduces the risk of graft migration. The stability of the graft is not a cause for concern.
Also, the reconstruction technique with LARS is a high-performance method, used especially in high-performance athletes, having the advantage of a much faster recovery and an almost non-existent recurrence rate.
After the operation, the patient must wear an orthosis, locked in full extension for 24 hours. There follows a recovery period, initiated in the hospital, then continued by the patient in a recovery center. Immobilization after surgery is no longer necessary today, we recommend an orthosis in the first month to prevent abnormal movements that may occur in the knee. If PCL reconstruction is associated with a meniscal suture, the use of the orthosis is all the more necessary.
Resumption of walking with support is early, in the days following the operation, using two crutches for several weeks (2-3). The duration of hospitalization varies from 24 to 48 hours.
Physical therapy begins quickly after surgery. It is done in our clinic and lasts 6 months, with 5 sessions per week.
The resumption of physical activities that do not require torsional movement is quite fast: it is the case of swimming and cycling that contribute to physical therapy in the first months after surgery. Long-distance walking can be resumed in the 3rd month. In contrast, other sports that require more anterior cruciate ligament can only be resumed after 6-9 months after surgery.
Possible complications after a PCL ligamentoplasty are fractures, popliteal artery lesions, deep vein thrombosis, residual laxity, and diminished range of motion. Residual laxity can be caused by additional, undiagnosed ligament injuries. An incomplete range of motion can be caused by the improper attachment of the graft or the application of too much tension, things that can be solved with the help of physical therapy or a new fixation.

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT