See details
READ MORE
Recovery protocol after Bankart intervention
Recovery after the restoration of shoulder instability through the Bankart procedure is not easy. The patient needs to understand that sometimes the recovery process is very difficult and can take a very long time. The patient must be very compliant with the treatment, patient and confident in the success of the treatment. He must perform daily recovery exercises to regain muscle strength and normal degrees of mobility. The complete recovery period cannot be anticipated and varies quite a lot. It normally lasts between 4 and 6 months, but sometimes it can last up to 12 months. Office work can be resumed 1 week after the surgical intervention, and physical activity is allowed after 6 months. The recovery period depends on the success of the surgery.At the end of the surgery, the patient is transferred from the operating room to the intensive care unit where he stays for a few hours. The operated limb is immobilized in a sling (special bandage), which the patient will wear continuously for 14 days, except when washing, dressing, and exercising. It is recommended that the patient sleep with the immobilization. The purpose of using this immobilization is to protect the suture or reinsertion of the joint capsule. After such an intervention in the next period, the patient will receive analgesics (pain medications), even if the literature describes bearable pain.
Cryotherapy is used postoperatively to reduce pain, local edema, muscle spasms and inflammatory response. Ice is used in rounds of 20-30 minutes in the first 4-5 days postoperatively.
After 2-3 days of hospitalization, the patient is discharged, going to see a doctor every 3 days until 14 days when the wires are removed. The patient will continue at home to take the medication prescribed by the attending physician: antibiotics and pain medications. It will continue with cryotherapy.

General considerations
- Postoperatively, the operated upper limb will be immobilized in a sling or shoulder orthosis.
- The following limb movements will be restricted for 4 weeks:
- Extension (in the back) beyond the body plane.
- External rotation (rotation of the limb outwards) over 0 (straight forward); extensive repairs may require more restrictions.
- Avoid any internal rotation.
- Avoid strong passive stretches to external rotation/extension for 3 months after a previous repair and internal rotation after a posterior repair.
- A correct position is vital during the recovery process because it ensures proper healing and reduces the risk of developing poor mechanics.
- Aerobic conditioning throughout the recovery process.
- All active exercises should be closely monitored to minimize substitution or compensation.
Week 1
Apply ice to the shoulder every 2 hours for 15-20 minutes during the day for 2 weeks.Manual:
- effleurage (a form of massage that involves circular and smooth movements made with the palm).
- mobilization of soft tissue around the muscles.
- slight scapular movements.
The home program consists of:
- elbow flexion / extension.
- strengthening the fist and forearm muscles.
- cervical stretching.
- postural education.
Objectives:
- Reduction of pain and edema.
- Initiation of passive range of motion with restrictions (Bankart anterior - without external rotation; Bankart posterior - without internal rotation).
- Passive range of motion <50 degrees flexion / abduction.
- The full extent of the elbow movement.
Week 2-4
Manual:- Effleurage.
- mobilization of soft tissue around the muscles.
- slight scapular movements.
- pain control (cryotherapy, massage, and electrical stimulation).
Objectives:
- Reduction of pain and edema.
- Passive range of motion <90 degrees flexion / abduction.
Week 4-6
Medical visit at 4 weeks and removal of the sling if the doctor recommends it.Manual:
- Mobilization of the tissue and muscles around the wound.
- Active and passive flexions assisted to the scapular plane.
- Active flexion of the arm against gravity to the scapular plane (within tolerability).
- No resistance until 30 repetitions can be performed with perfect mechanics.
- Isotonic exercises of the fist, forearm, and scapula.
- Pulling exercises of the upper limb to the front and from the scapular plane.
- Elbow flexion.
- Submaximal isometric exercises (up to the limit dictated by pain).
- Active exercises for lifting and retracting the scapula.
- Allowed to carry light weights.
- Exercises on the ergometer without resistance or with minimum resistance.
- Proprioceptive training begins (writing the alphabet, fine motor skills, exercises specific to the service/sports activity practiced).
Objectives:
- Removing the sling; minimal pain at rest.
- Initiation of the active scope of the flexion and abduction movement.

Week 6-8
Manual:- Continue to mobilize the soft tissue and improve the range of motion.
Exercises:
- Continue the progression of the range of motion within the tolerability limit (anterior tooth, upper and lower trapezius); add eccentric exercises.
- You can start a slight stretch to external rotation.
- Easy mobilization of the glenohumeral joint can begin.
- Easy internal rotation exercises from 0 degrees to the body can be added.
- Progression of proprioceptive training (bent at the elbows, quadruple / "hands and knees" position for rhythmic stabilization).
- Exercises on the ergometer with increasing resistance.
- Movement range greater than 80% of normal, initiate hand movements behind the head, back exercises within tolerability.
- Start jogging, cycling, arm lifting exercises against resistance in the pool.
Week 8-12
- The emphasis is on regaining strength and endurance.
- Active exercises of range of motion, including internal and external rotation, arm abduction, press.
- Running, road, or mountain biking; no activity with forced, ballistic arm movements.
3-6 Months:
- Medical visit at 12 weeks.
- Aggressive extension; starting exercises with intense resistance.
- Adding easy throwing exercises with attention focused on proper mechanics.
6 months:
- You can intensify the throwing exercises.

NB: All progressions are approximations and should only be used as guidance. Progression will be based on the individual condition of the patient, which is assessed throughout the treatment process.
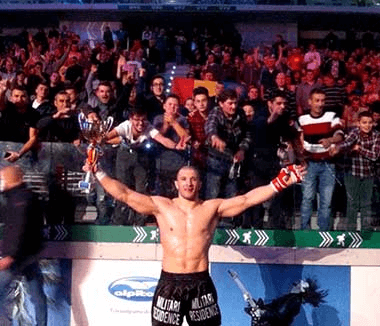
SUCCESSFUL RECOVERY STORIES

MAKE AN APPOINTMENT
CONTACT US
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT