See details
READ MORE
Article written by Dr. Alizzi Khalid, recovery practitioner, with over 10 years of experience in rheumatology.
General information about osteoporosis
Osteoporosis is an extremely common condition that causes the bones to become weak and fragile - so fragile that a fall or even slight stress, such as bending or coughing, can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist, or spine.Bones are living tissues that are constantly affected and replaced. Osteoporosis occurs when the creation of new bone does not keep pace with the removal of old bone. Osteoporosis affects men and women of all races. White and Asian women - especially older women who have gone through menopause - are at the highest risk. Medications, a healthy diet, and exercise can help prevent bone loss or strengthen already weak bones.
What is osteoporosis
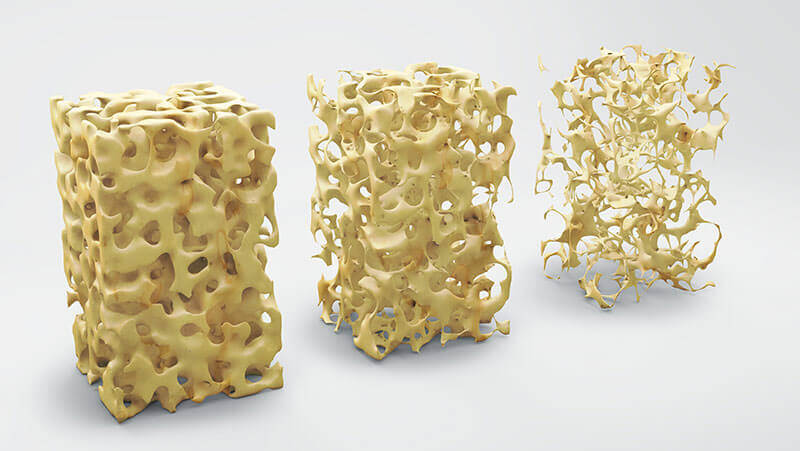
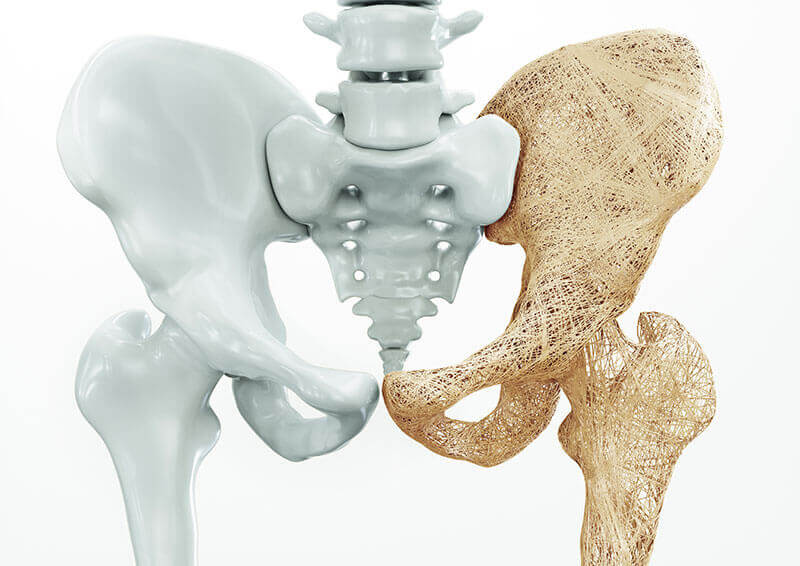
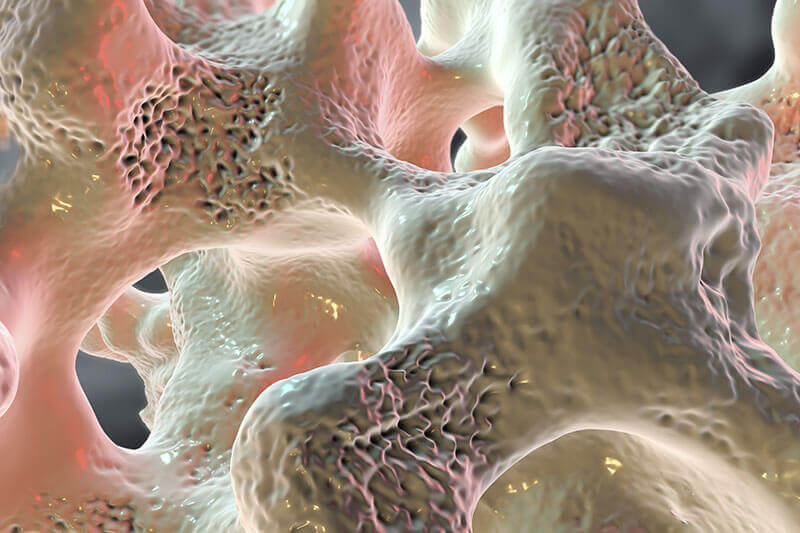
Osteoporosis is a condition characterized by a decrease in bone density, reducing its strength and resulting in fragile bones. Osteoporosis leads to an abnormal porous bone that is compressible, like a sponge. This skeletal disorder weakens the bone and leads to frequent bone fractures.Osteoporosis means "porous bone". Seen under a microscope, the healthy bone looks like a honeycomb. When osteoporosis occurs, the holes and spaces in the honeycomb are much larger than in healthy bone. Osteoporotic bones lose their density or mass and contain abnormal tissue structures. As the bones become less dense, they weaken and are more likely to break.
Normal bones are made up of protein, collagen, and calcium, all of which give the bones strength. Bones affected by osteoporosis can rupture (fracture) with relatively minor injuries, which would not normally cause a bone to rupture. The fracture can be either in the form of a crack (as in the case of a hip fracture) or collapse (as in the case of a compression fracture of the vertebral column). The spine, hips, ribs, and wrists are common areas of bone fractures from osteoporosis, although osteoporosis-related fractures can occur in almost any skeletal bone.
Causes of osteoporosis
Osteoporosis occurs when there is an imbalance between new bone formation and old bone resorption. Two minerals essential for normal bone formation are calcium and phosphate. Throughout youth, the body uses these minerals to produce bones. Calcium is essential for the proper functioning of the heart, brain, and other organs. To keep the critical organs functional, the body reabsorbs the calcium stored in the bones to maintain the level of calcium in the blood. If calcium intake is not enough or if the body does not absorb enough calcium from the diet, bone production and bone tissue may suffer. Thus, the bones may become weaker, resulting in fragile bones that can break easily. The major cause of osteoporosis is the lack of certain hormones, especially estrogen in women and androgen in men. Women, especially those over the age of 60, are frequently diagnosed with this disease. Menopause is accompanied by lower estrogen levels and increases a woman's risk of developing osteoporosis. Other factors that can contribute to bone loss in this age group include insufficient intake of calcium and vitamin D, lack of weight exercise, and other age-related changes in endocrine function (in addition to lack of estrogen).
Other conditions that can lead to osteoporosis include excessive use of corticosteroids (Cushing's syndrome), thyroid problems, lack of muscle use, bone cancer, certain genetic disorders, use of certain medications, and problems such as low calcium in the diet. Other conditions that can lead to osteoporosis include excessive use of corticosteroids (Cushing's syndrome), thyroid problems, lack of muscle use, bone cancer, certain genetic disorders, use of certain medications, and problems such as low calcium in the diet.
Symptoms of osteoporosis
The early stages of osteoporosis do not cause symptoms or warning signs. In most cases, people with osteoporosis do not know they have this condition until they have a fracture.If symptoms occur, some of the earliest may include:
- weak grip
- weak and fragile nails
Later, during the illness, sharp pains may appear suddenly. The pain may not radiate (spread to other areas); it can be aggravated by an activity that puts weight on the area, can be accompanied by sensitivity, and generally begins to decrease within a week. But there are cases where the pain can last over three months.
Types of osteoporosis
There are four types of osteoporosis: primary, secondary, imperfect osteogenesis, and idiopathic juvenile.Primary osteoporosis
Primary osteoporosis is the most common type of osteoporosis. It is more common in women than in men. A person reaches maximum bone mass (density) at about 30 years of age. After that, the rate of bone loss increases slowly, while the rate of bone construction decreases. Whether a person develops osteoporosis depends on the thickness of the bones at the beginning of life, as well as health, diet, and physical activity at all ages.
Primary osteoporosis is the most common type of osteoporosis. It is more common in women than in men. A person reaches maximum bone mass (density) at about 30 years of age. After that, the rate of bone loss increases slowly, while the rate of bone construction decreases. Whether a person develops osteoporosis depends on the thickness of the bones at the beginning of life, as well as health, diet, and physical activity at all ages.
Secondary osteoporosis
Secondary osteoporosis has the same symptoms as primary osteoporosis. But it occurs as a result of medical conditions, such as hyperparathyroidism, hyperthyroidism, or leukemia. It can also occur as a result of the administration of known drugs that cause bone destruction, such as oral or high-dose inhaled corticosteroids (if used for over 6 months). Secondary osteoporosis can occur at any age.
Imperfect osteogenesis
Imperfect osteogenesis is a rare form of osteoporosis that can occur even in the womb, but most cases are diagnosed after birth. Imperfect osteogenesis causes bones to rupture for no apparent reason.
Idiopathic juvenile osteoporosis
Idiopathic juvenile osteoporosis is rare. This happens in children aged between 8 and 14 years or in periods of rapid growth. There is no known cause for this type of osteoporosis, in which there is too little bone formation or excessive bone loss. This condition increases the risk of fractures.
The diagnosis of osteoporosis can be easily made by Dr. Alizzi Khalid :
To check for osteoporosis, your doctor will review your medical history and perform a physical exam. Blood and urine tests can also be performed to check for conditions that may cause bone loss. If your doctor considers that you may have osteoporosis or that you are at risk of developing osteoporosis, he or she may suggest a bone density test.
This painless test lasts between 10 and 30 minutes.
Traditional radiographs cannot measure bone density, but they can identify fractures of the spine. More specialized techniques must measure bone mineral density. Several types of tests are available, but the most commonly used is DXA (double energy X-ray absorption). DXA is a low-radiation test that can detect relatively small percentages of bone loss. It is used to measure the density of the bone in the spine and hip and can also measure the bone density of the entire skeleton. There are several types of testing options:
- DXA (peripheral DXA) measures bone mass in the forearm, finger, and heel.
- SXA (single energy X-ray absorptiometry) measures the heel or wrist.
- DPA (dual photon absorption) measures the spine, hip, or entire body.
- SPA (single photon absorptiometry) measures the wrist.
- QCT (Quantitative Computed Tomography) measures the spine or hip
- PQCT (peripheral QCT) measures the forearm.
- QUS (Quantitative Ultrasound) uses sound waves to measure your heel or finger.
- Women are at higher risk than men, especially women who are thin or have a small frame, as well as the elderly.
- Women who are white or Asian, especially those with a family member with osteoporosis, have a higher risk of developing osteoporosis than other women.
- Postmenopausal women, including those who have caused early or surgical menopause, are at higher risk.
- Smoking, eating disorders such as anorexia nervosa or bulimia, low dietary calcium, alcohol consumption, inactive lifestyle, and the use of certain medications, such as corticosteroids and anticonvulsants, are also risk factors.
- Rheumatoid arthritis itself is a risk factor for osteoporosis.
- Having a parent who has had osteoporosis is a risk factor for offspring.

Improving the effects and managing osteoporosis
Sfaturile Dr. Alizzi Khalid: in osteoporoza, este important sa se previna caderile si fracturile. Dar asta nu inseamna sa stati pe margine. Poate fi o provocare in gasirea unui echilibru intre ingrijirea sanatatii dumneavoastra si a nu deveni izolat, mai ales daca acest lucru inseamna ca evitati activitati si interese care sunt importante pentru dumneavoastra. Va puteti gandi la osteoporoza ca un diagnostic care va solicita sa luati decizii informate cu privire la schimbarile de stil de viata, si tratamente eficiente cu medicamente care va vor reduce riscul de fracturi in viitor. Caldura, masajul, medicamentele analgezice si odihna pot ameliora efectele osteoporozei. Drug treatment for osteoporosis
Dr. Alizzi Khalid's advice: In osteoporosis, it is important to prevent falls and fractures. But that doesn't mean sitting on the sidelines. It can be a challenge to find a balance between taking care of your health and not becoming isolated, especially if this means avoiding activities and interests that are important to you. You can think of osteoporosis as a diagnosis that requires you to make informed decisions about lifestyle changes, and effective treatments with medications that will reduce your risk of fractures in the future. Heat, massage, painkillers, and rest can alleviate the effects of osteoporosis. The drugs are used both to prevent and treat osteoporosis. Some medications slow down the rate of bone loss or increase bone thickness. Even small amounts of new bone growth can reduce your risk of bone deformity.
Bisphosphonates . These include alendronate (Fosamax), ibandronate (Boniva), risedronate (Actonel) and zoledronic acid (Reclast).
Calcitonin (Calcimar or Miacalcin). This is a natural hormone that helps regulate the level of calcium in your body and is part of the process of building bones. Calcitonin also relieves pain caused by compression fractures of the spine.
Denosumab (Prolia). It is used to treat people who have an increased risk of bone fractures related to decreased bone density.
Teriparatide(Forteo). It is used to treat men as well as postmenopausal women who have severe osteoporosis and are at increased risk of bone fractures.
Raloxifen (Evista). This drug is a selective modulator of estrogen receptors.
Hormone therapy is not usually recommended for most women with osteoporosis. But if you are at high risk and cannot take other medicines, your doctor may recommend it in certain circumstances.
Surgical procedures for osteoporosis
Vertebroplasty is a minimally invasive procedure used to strengthen vertebrae with compression fractures, which are common in patients with osteoporosis. Vertebroplasty involves injecting an acrylic compound into the collateral vertebrae to stabilize weakened bones. The procedure is performed in an operating room or a radiology suite, and the treatment of each affected vertebra lasts about an hour. Local anesthesia is injected into the vertebra, a small incision is made and a bone biopsy needle is inserted. Several small syringes of cementitious material are then injected through the needle into the vertebra. The cement hardens almost immediately.Multiple compression fractures of the spine caused by osteoporosis can lead to loss of height, kyphosis (extreme curvature of the spine), and pain. Kyphoplasty, also called balloon kyphoplasty, is a minimally invasive procedure used to restore vertebral height and stabilize weakened bone. Kyphoplasty cannot correct spinal deformities and is used in patients who have had recent fractures (within 2-4 months). The procedure is usually performed in a hospital under local or general anesthesia and takes about an hour for each vertebra affected.
In balloon kyphoplasty, a small incision is made and a fluoroscope (a device comprising a screen and an X-ray tube) is used to guide the insertion of a balloon catheter into the vertebra. The balloon is slowly inflated to lift the compressed vertebra and then deflated. An acrylic compound (cementitious material) is then injected into the vertebra through a bone biopsy needle. The material hardens almost immediately. Pain reduction usually occurs in 2 days.
Most patients are discharged from the hospital the second day after kyphoplasty and can resume daily discharge activities. Intense activity, such as heavy lifting, should be avoided for at least 6 weeks.
Complications of kyphoplasty are rare and include:
- Adverse reaction to anesthesia
- The cementing material can drain into the veins or the epidural space around the vertebrae
- Nerve damage
- Spinal cord injuries
Natural Treatment for Osteoporosis
Some people may need medication for severe bone disorders. Even if you decide to take medication, the natural approach can provide clear and long-lasting benefits. You can opt for the application of essential oils in painful areas, to increase bone density and try aromatherapy.
Two other vital things you need to consider improving bone density are exercise and sun exposure.
Weightlifting 3 times a week for 30 minutes and 20 minutes of daily sun exposure can help relieve the pain caused by osteoporosis. Also, standing on vibrating platforms for 5-20 minutes a day can improve bone density.
The natural supplements recommended by Dr. Alizzi Khalid are:
- Magnesium (500 mg daily) - Magnesium is needed for proper calcium metabolism.
- Calcium (1000 mg daily) - Choose calcium citrate that is best absorbed.
- Vitamin D3 (5,000 IU per day) - Vitamin D helps improve calcium absorption.
- Vitamin K2 (100 mcg per day) - It is needed to form protein critical for bone formation. Take high-quality vitamin K2 supplements, or eat more foods rich in vitamin K.
- Strontium (680 mg daily) - May help improve bone density.
Spas recommended for osteoporosis patients
Spas are indicated according to health problems and the properties of therapeutic waters. Saltwater and sapropelic mud have anti-inflammatory properties and are indicated for people suffering from osteoporosis or who have suffered bone injuries. The spa resort Ocna Sugatag is famous for its healing properties, the spa resort Valea Stelii has two saltwater pools, the salt lakes of Sovata are formed by salt ponds in small or large depressions, and the most important is Lake Ursu and Lake Negru.The spa resort Ocna Sibiului is more and more requested, having high concentration salt waters, and slightly mineralized sapropelic mud.
Nutrition in osteoporosis
The most important nutrients for people with osteoporosis are calcium and vitamin D. Calcium is a key element for your bones. Vitamin D helps the body absorb calcium.The goal is to eat meals that include a wide variety of foods from the four major groups. These are fruits and vegetables; carbohydrates such as bread, potatoes, pasta, and cereals; dairy and alternative products; beans, fish, eggs, meat, and other proteins. The food for your bones doesn't have to be boring; there are plenty of delicious meals and snacks full of vitamins and minerals you need.
- Eat plenty of whole foods, such as brown rice.
- Eat more fruits and vegetables; at least five servings a day. Choose different colored fruits and vegetables to make sure you have the range of essential nutrients you need, including calcium.
- Eat more fish; Try two servings a week and remember that fatty fish, such as mackerel, are also an excellent source of vitamin D.
- Reduce saturated fats and sugar. Check food labels: 5g or more of saturated fat per 100g and 10g or more of sugar per 100g means a lot.
- Try to reduce the amount of salt you consume. Again, check food labels and remember that 0.5g or more of sodium per 100g means a lot.
- Don't skip breakfast. If you are not hungry when you wake up, start with a healthy snack and eat regular meals throughout the day to maintain your health and well-being.
The benefits of physiotherapy for osteoporosis
Physical therapy can be incorporated into the treatment plan. Physical therapy can help the patient build strength, flexibility, and increase range of motion. Exercise promotes circulation that stimulates bones to heal and strength builds balance, which can help prevent falls. During physical therapy, the patient is taught "safe" movements to prevent injuries. The therapist can offer a personalized exercise program.What you do in physical therapy depends a lot on you: the cause of osteoporosis, the level of physical activity, the level of risk for spinal fractures, and what your body can do. However, your physical therapist will work with you to develop an exercise plan that involves weight exercises (such as walking or tennis) and strengthening exercises (such as lifting weights).
Depending on your needs, the physical therapist can also work on your balance and position. The improved balance will help you prevent falling. Posture is important throughout life, but it is especially important if you have or could have osteoporosis. Poor posture can mean that the upper back is more rounded than it should be. A rounded back puts more pressure on the spine, increasing the risk of spinal fractures. The more you lean, the more likely you are to fall.
The physical therapist can also teach you alternative ways to safely engage in "daily activities," such as getting out of bed or sitting. With weak bones, these activities can be challenging, and if you fall, you can fracture a bone.
Recommended exercise to prevent accidents associated with osteoporosis
Being active is a powerful medicine for people with osteoporosis. Exercise helps slow down bone loss and build stronger muscles to support you so that you are less likely to fall or break a bone. But not every workout will help. If you can, do things that strengthen your muscles and do some weight-bearing exercises. This means that your feet will support you as you move. Because gravity puts stress on the bones, they build more cells. These exercises include any movement while standing. If you have severe osteoporosis or have already had a broken bone or fracture, some activities can be risky.
Many studies have shown that people with better posture, better balance, and greater muscle strength are less likely to fall and are therefore less likely to be injured.
The study shows that women over the age of 80, with an individually tailored exercise regimen that incorporates progressive muscle strengthening, balance training, and a walking plan, can reduce their overall risk of falling by about 20% over 30%.
Having a good posture is important and can help you avoid stress on your spine. Good posture involves keeping your head straight, chin forward, shoulders back, upper back, and arched lower arch. To practice good standing:
- Stand with your head and shoulders leaning against a wall, with your heels two to three inches from the wall.
- Pull your chin forward and tense your abdomen.
- Press your back against the wall, leaving a small space between the wall and the curvature of your back.
Exercises for balance
One study found that patients who practice Tai Chi, a Chinese exercise focused on balance, are 50 percent less likely to fall or injure than those who do not. This significant improvement was achieved after only 15 weeks, during which patients received one Tai Chi lesson per week with an instructor, and were asked to practice twice a day for 15 minutes on their own.Exercises to increase flexibility
Get flexibility with Yoga
Don't be fooled by its gentle nature - besides helping you in position and flexibility, it will also strengthen your bones. Some positions, especially forward bending, may not be suitable for people with osteoporosis.
Rotating the joints through their full range of motion will help you maintain muscle function. Stretching is best done after warming up the muscles - for example, at the end of the exercise session or after a 10-minute warm-up. These should be done easily and slowly, without jumping.
Avoid stretching that flexes your spine or causes you to bend at the waist.
Strength training helps strengthen the muscles and bones in the arms and upper spine, and weight-bearing exercises - such as walking, jogging, running, climbing stairs, jumping rope - help especially the bones in the legs, and lower spine.
Work with weights
This will build bones and strengthen muscles at the same time. The goal is to focus on each major muscle group twice a week, with at least one day of rest between workouts. If you are new to lifting weights, consult your doctor first and work with a coach to see which exercises are right for you.
Preventing osteoporosis through a healthy lifestyle
Good nutrition and regular exercise are essential for maintaining healthy bones throughout life.Protein
Protein is one of the basic components of bone. And while most people get a lot of protein in their diet, others are missing out. Vegetarians and vegans can get enough protein in their diet if they intentionally seek out appropriate sources, such as soy, nuts, legumes, dairy, and eggs if allowed. Older adults may also consume less protein for a variety of reasons. Protein supplementation is an option.Bodyweight
Underweight increases the chances of bone loss and fractures. Excess weight is now known to increase the risk of fractures in the arm and wrist. Thus, maintaining proper body weight is beneficial for the bones, as well as for health in general.Calcium
Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70. Excellent sources of calcium include:- Low-fat dairy products
- Vegetables with green leaves
- Canned salmon or sardines with bones
- Soy products such as tofu
- Cereals fortified with calcium and orange juice
Nutrition
Getting enough calcium and vitamin D is one of the first steps in preventing or reducing the effects of osteoporosis. Vitamin D helps the body absorb calcium. Calcium is found in many foods, including dairy products such as milk and yogurt.
Exercise and exercise
Exercise plays an important role in building and maintaining bone and muscle strength. It also helps reduce falls by improving balance and helps rehabilitate fractures. Muscles and bones respond and strengthen when they are "stressed." This can be done through weight-bearing or impact exercises.
Why exercise is vital for bone and muscle health:
Build strong bones in youth. It is estimated that a 10% increase in peak bone mass in children may reduce the risk of an osteoporotic fracture during adulthood by 50%.Exercise plays a key role in adults, preventing bone loss, and maintaining muscle strength. It helps prevent weak bones and falls in the elderly. One-third of people over the age of 65 have a fall each year, and the risk of falling increases with age.
People who have suffered fractures can benefit from special exercises and training (under medical supervision) to improve muscle strength and muscle function, for greater mobility and improved quality of life.
Outdoor activities and vitamin D
Vitamin D is essential for the development and maintenance of bone, both for its role in assisting the absorption of calcium from foods in the intestine and for ensuring the proper renewal and mineralization of bone tissue. The type of vitamin D produced in the skin is called vitamin D3 (cholecalciferol), while the dietary form may be vitamin D3 or a molecule of similar plant origin, known as vitamin D2 (ergocalciferol).Sources of Vitamin D
Vitamin D is produced in the skin when exposed to ultraviolet B rays; in children and adults, exposure of the hands, face, and arms to the sun for 10 to 15 minutes a day is usually sufficient for most people. However, how much vitamin D is produced by sunlight depends on the time of day where you live in the world and the color of your skin. Vitamin D can also be obtained from foods and dietary supplements. Food sources are quite limited and include oily fish, such as salmon, sardines and mackerel, eggs, liver, and dairy foods and grains.
The ideal combination is to perform physical exercises or walks outdoors because this way you also benefit from exercise and at the same time you are loaded with vitamin D from the sun's rays.
IN CASE YOU HAVEN'T ALREADY HEARD ABOUT US
Centrokinetic is the place where you will find clear answers and solutions for your motricity problems. The clinic is dedicated to osteoarticular diseases and is divided into the following specialized departments:
Orthopedics , a department composed of an extremely experienced team of orthopedic doctors, led by Dr. Andrei Ioan Bogdan, primary care physician in orthopedics-traumatology, with surgical activity at Medlife Orthopedic Hospital, specialized in sports traumatology and ankle and foot surgery.
Pediatric orthopedics , where children's sports conditions are treated (ligament and meniscus injuries), spinal deformities (scoliosis, kyphosis, hyperlordosis) and those of the feet (hallux valgus, hallux rigidus, equine larynx, flat valgus, hollow foot).
Neurology , which has an ultra-performing department, where consultations, electroencephalograms (EEG) and electromyography (EMG) are performed.
Medical recovery for adults and children , department specialized in the recovery of performance athletes, in spinal disorders, in the recovery of children with neurological and traumatic diseases. Our experience is extremely rich, treating over 5000 performance athletes.
Medical imaging , the clinic being equipped with ultrasound and MRI, high-performance devices dedicated to musculoskeletal disorders, and complemented by an experienced team of radiologists: Dr. Sorin Ghiea and Dr. Cosmin Pantu, specialized in musculoskeletal imaging.
Find the latest news by following the Facebook and YouTube accounts of the Centrokinetic clinic.

MAKE AN APPOINTMENT
CONTACT US
SUCCESSFUL RECOVERY STORIES
MAKE AN APPOINTMENT
FOR AN EXAMINATION
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT