Myelitis: what it is, causes, symptoms, and treatment options
.jpg)
Myelitis is a rare problem that can cause severe symptoms and, in some cases, can lead to severe complications such as partial or complete paralysis. Continue reading to learn more about myelitis, its causes and symptoms, and the available treatment options!
What is myelitis?
Myelitis refers to inflammation of the spinal cord, a vital component of the nervous system that transmits signals from the brain to the rest of the body, thus controlling motor, sensory, and autonomic functions. This inflammation can damage myelin, a substance that protects nerves and helps transmit signals quickly.[1][3]
Types of myelitis
Myelitis is a complex condition that presents in various forms, classified according to the affected area or the cause of the inflammation. The most common type is transverse myelitis, an inflammation that affects both sides of a specific section of the spinal cord.[1][3]
Other types of myelitis include:
- acute flaccid myelitis;
- poliomyelitis;
- meningomyelitis;
- leukomyelitis.[1][2][3]
Causes of myelitis
The causes of myelitis are multiple and cannot be identified with certainty in every case, but viral, bacterial, and fungal infections, as well as various inflammatory and autoimmune conditions, can be involved.
Examples of viral infections that can lead to the development of myelitis include:
- herpes viruses (including the one that causes chickenpox and shingles);
- Cytomegalovirus infection;
- Epstein-Barr virus infection;
- HIV infection;
- enterovirus infections such as poliovirus and Coxsackie virus;
- West Nile virus infection;
- Zika virus infection;
- influenza;
- hepatitis B.[1][3]
Bacterial causes of myelitis can include:
- Lyme disease;
- syphilis;
- tuberculosis;
- pertussis (whooping cough);
- tetanus;
- gastroenteritis;
- bacterial pneumonia.[1][3]
The list of inflammatory and autoimmune conditions associated with myelitis includes:
- multiple sclerosis, in which the immune system destroys the myelin around the nerves in the spinal cord and brain;
- neuromyelitis optica (Devic's disease), which causes inflammation and loss of myelin around the spinal cord and the eye nerve that transmits information to the brain;
- lupus, which can affect multiple systems of the body;
- Sjögren's syndrome, which causes severe dryness of the mouth and eyes.[1][3]
In rare cases, myelitis can occur after certain vaccinations.[1][3]
Symptoms of Myelitis
.jpg)
The symptoms of myelitis can vary considerably depending on the type and severity of spinal cord inflammation. In the case of transverse myelitis, for example, the most commonly observed symptoms include:
- weakness in the legs and arms;
- lower back pain or sharp pains that radiate down the legs or arms, or around the torso;
- paresthesia;
- bowel and bladder dysfunction (e.g., frequent need to urinate, incontinence or urinary retention, and constipation).[1][3]
In the case of acute flaccid myelitis, sudden onset of weakness in the arms or legs, loss of muscle tone, and loss of reflexes are the most common symptoms. Other possible symptoms include:
- difficulty moving the eyes;
- drooping eyelids;
- facial weakness;
- difficulty swallowing;
- slurred speech;
- pain in the arms or legs;
- neck or back pain.[2]
In less common cases, affected individuals may also experience numbness or tingling in the arms or legs.[2]
Diagnosis of Myelitis
The diagnosis of myelitis is based on both the patient's medical history and a thorough neurological examination. These are essential to determine whether the patient suffers from this condition and to exclude or evaluate other possible causes.
Several tests are used to confirm or rule out the presence of myelitis. Magnetic resonance imaging (MRI) is considered very effective in detecting lesions in the spinal cord, a sign of myelitis. A brain MRI can also provide valuable information about other possible underlying causes, such as multiple sclerosis.[1][3]
Blood tests can identify or rule out certain disorders, including HIV infection or vitamin B12 deficiency. Lumbar puncture and cerebrospinal fluid analysis are other diagnostic methods that can reveal the presence of infections, increased protein levels, or a high number of white blood cells (leukocytes) – the latter being signs of a body fighting an infection.[1][3]
Treatment Options for Myelitis
Treatment for myelitis is tailored according to the severity and type of the disease, with options ranging from medications to physical therapy or various procedures. The main goal of these treatments is to reduce symptoms, improve the patient's quality of life, and prevent complications.[1][3]
Regarding medications used to treat myelitis, these can include corticosteroids, which are intended to reduce inflammation, immunosuppressive drugs to slow down the activity of the immune system, and medications to relieve specific symptoms such as pain. Other treatments for myelitis may include intravenous immunoglobulin, which helps modulate the faulty immune response leading to inflammation, and plasmapheresis, which removes abnormal antibodies from the plasma that are thought to attack nerve cells.[1][3]
Physical therapy plays an essential role in the treatment of myelitis. It involves exercises designed to improve strength and coordination, preventing muscle atrophy and improving mobility. In addition to physical therapy, occupational therapy can also be beneficial. This involves training the patient to perform daily activities and reintegrate socially and professionally. Occupational therapists work closely with patients to help them adapt to the changes caused by the disease and maintain the best possible quality of life.[1][3]
It is important to note that each patient is unique and requires an individualized treatment plan. Consultation with a specialist physician is essential to determine the best course of action.
Recovery from myelitis varies significantly from person to person. Some people recover completely, while others may be left with permanent disabilities. Factors that can influence the prognosis include the severity of the condition, the age at which it occurs, and the patient's overall health.[1][3] It is important to note that the information presented in this article is for informational purposes only and does not replace specialist medical advice. If you suspect that you or someone you know may have myelitis, it is essential to consult a doctor for a correct diagnosis and appropriate treatment plan!
Bibliography:
- „Transverse Myelitis”, Mayo Clinic, 2022. Accessed June 4, 2024.
- „About Acute Flaccid Myelitis (AFM)”, Centers for Disease Control and Prevention, June 10, 2022. Accessed June 4, 2024.
- „Transverse Myelitis (TM): Causes, Symptoms & Treatment”, Cleveland Clinic, 2022. Accessed June 4, 2024.
BUCHAREST TEAM
CLUJ NAPOCA TEAM
BRASOV TEAM
MAKE AN APPOINTMENT
FOR AN EXAMINATION
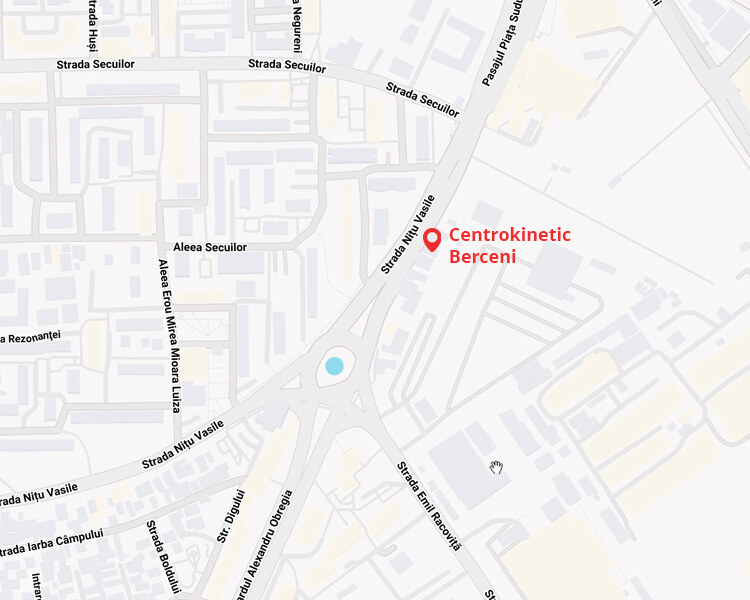
See here how you can make an appointment and the location of our clinics.
MAKE AN APPOINTMENT